Authors
Content
Foreword
By Rt Hon Sajid Javid MP
Secretary of State for Health and Social Care (2021-2022)
Twelve months ago, I announced to Parliament that a concerning new variant of Covid-19 had been detected overseas. The sequence B.1.1.529, better known now as Omicron, was probably already on our shores and would very likely go on to infect millions of people.
As had been the case throughout the pandemic, we faced a race between the vaccine and the virus. Within weeks, the total number of boosters delivered reached 35 million. On a single day in December, over 1 million Covid-19 jabs were administered.
Severe restrictions avoided, and thousands of lives saved. All due to vaccination and our pharmaceutical defences.
There is much we can learn from the past two years. For vaccination policy, the challenge is to create a sustainable framework both in the face of future public health emergencies, and the need to help build a healthier population.
Helping to build that population requires a long-term focus on prevention. This country had been at the cutting edge of health improvement in the past. But the pandemic shone a light on the critical issues we face today. We know that poor health, exacerbated by severe disparities across the country, is not just economically destructive, but socially unjust.
We must not shy away from this. Fortunately, we have the tools available to improve health outcomes and vaccination is amongst the most effective. We are now capable of vaccinating against more than a dozen preventable diseases across people’s lives. This not only enriches the lives of individuals, but our economy as a whole – as well as relieving pressure on public services.
The case for strengthening our national vaccination policy is therefore extremely strong and this report offers some credible and important ideas to make this a reality. This excellent report offers several notable pointers:
First, the development of better immunisation infrastructure at a national and local level. This will not only help to expand the offer of vaccination to communities– but provide the UK much needed resilience to tackle future health challenges.
Second, the use of digital technology and data. We must look at the huge advances of the pandemic, not just as a quirk of history, but the start of a new era of digital transformation, and a platform upon which to build. By enabling the responsible flow of data around the system in vaccination policy, we can better inform and refine our strategies to encourage uptake.
Third, it is clear we should be making better use of our wider workforce – including capable volunteers and medical and nursing students to support our seasonal rollouts. This needs to be planned with care to complement the expertise of our practice nurses, GPs and pharmacists.
The fragility of disease control means that I will sadly not be the last Health Secretary to stand at the Despatch Box and announce the spread of a concerning new disease. It is because we know this is inevitable, that we must do more now to strengthen our health infrastructure.
As a Conservative, I believe that we have a responsibility to preserve and replenish the health of the nation. We are in a strong position to do this and possess a historic global leadership position in vaccination. We must do all we can to keep it.
Next chapterEndorsements
“COVID-19 reminded us all of the vital role vaccination plays in protecting our health. With many new vaccines currently in development, this report offers a wealth of credible ideas to ensure the UK is well placed to deliver the vaccines of the future to those who need them. It includes practical measures to strengthen the important work of JCVI, support front-line immunisation teams and create new ways for people to be vaccinated at a time and place that suits them.”
Dr Richard Torbett, Chief Executive, The Association of the British Pharmaceutical Industry
“In a challenging time for health and social care services, the Covid-19 vaccine is one example of how building partnerships in local communities and listening to people’s concerns resulted in an efficient and successful roll-out of a health intervention. This important research builds on that model, suggesting the best way to improve take-up of key preventative vaccines is by giving more power to local providers working in partnership with pharmacies and communities. It also suggests making better use of the NHS app to support vaccination bookings and records, something we know makes people feel more empowered and in control of their own health. Vaccines are an essential part of preventative health, underpinning an effective national health system, and it’s important we don’t lose sight of maintaining and improving public trust and take-up through the strategies this research recommends.”
Louise Ansari, National Director, Healthwatch England
“As a former DPH, I warmly welcome this comprehensive and visionary report from Policy Exchange which builds on the lessons learnt from the long experience of implementing immunisation, recognises the challenges facing local authority public health teams, especially in terms of investment, but highlights their critical role in strengthening the resilience of the nation’s health protection system through their statutory role in boroughs working with a wide range of stakeholders to protect the health of their populations. The report’s progressive and practical recommendations should be considered carefully by policymakers not least because of their timeliness with WHO warning that measles is now an imminent global threat following the pandemic and currently, in England, where vaccination rates have dropped to their lowest in a decade. There is a pressing need to take urgent action to ensure English immunisation policies, systems and services can respond effectively, rapidly and flexibly to those challenges and the recommendations offer the possibility of making that happen from the practical steps to create a flexible wider public health workforce, timely, robust shared digital surveillance systems and data reporting and the strengthening and reform of JCVI and setting up of a National Immunisation Board. This important report is a must read and its recommendations if acted upon will implement the lessons from the pandemic and ensure that England has an immunisation system not just fit for today but fit for the future”
Professor Kate Ardern, Former Director of Public Health, Wigan Council; Former Lead Director for Health Protection, Greater Manchester Combined Authority & Honorary Professor of Public Health, Salford University
“This timely and thorough report from Policy Exchange acknowledges the important role public health teams across the country play in supporting vaccination efforts and profiles some of the innovative ways that local government has partnered with the NHS to drive uptake in recent years. We welcome the measures proposed which look to foster greater cooperation between providers at a local level, and think the proposal to establish ‘Vaccine Collaboratives’ is worth further consideration. We were particularly pleased to see our call for a Memorandum of Understanding and Framework Agreement between UKHSA and the LGA also advocated in this report to strengthen links between national and local decision-makers”.
Councillor David Fothergill, Chair, Local Government Association Community Wellbeing Board
“I welcome this report from Policy Exchange which recognises the vital contribution of pharmacy teams in supporting flu and COVID-19 vaccination programmes each year and in engaging local communities to reduce vaccine hesitancy. Driving vaccine uptake across the life course will require concerted effort across Government and the NHS. It is heartening therefore to see proposals which look to encourage the conditions for community pharmacy to do more, with proposals to commission pharmacy to deliver more adult vaccines, measures to boost the vaccination workforce and to improve information sharing between providers across primary care so that ‘opportunistic’ vaccination can be more easily achieved. We hope many of these practical proposals are taken forward.”
Thorrun Govind, English Pharmacy Board Chair, Royal Pharmaceutical Society
“We welcome this timely report which recognises the important – and growing – contribution that community pharmacy plays in delivering national vaccination programmes. We have long campaigned for community pharmacies to be the natural home for all vaccinations. From commissioning community pharmacy to administer more vaccinations, enabling pharmacy technicians to administer them and improving accessibility to patient records – Policy Exchange has produced a range of credible ideas here which ought to be taken forward”
Malcolm Harrison, Chief Executive of the Company Chemists’ Association
“The Royal Society for Public Health welcomes this new report from Policy Exchange which draws upon insights from own work on measures to promote vaccination uptake across the life course as well as the perspectives of a wide range of public health professionals. The result is a credible set of policy solutions which ought to be taken forward. In particular, we are pleased to see an emphasis on measures to tailor campaigns to meet the specific needs of communities (particularly those that are underserved) and to leverage opportunities to engage a new generation of public health professionals through immunisation activities.”
Dr Jyotsna Vohra, Director for Policy and Communications, Royal Society for Public Health
Next chapterExecutive Summary
“Will it make the boat go faster?” That was the challenge that a group of British rowers set themselves when they agreed a target to achieve an Olympic Gold in the Sydney 2000 Olympics. Each possible innovation would be tested through this prism. If it helped the boat go faster, it was kept. Anything which slowed progress was dispensed with.
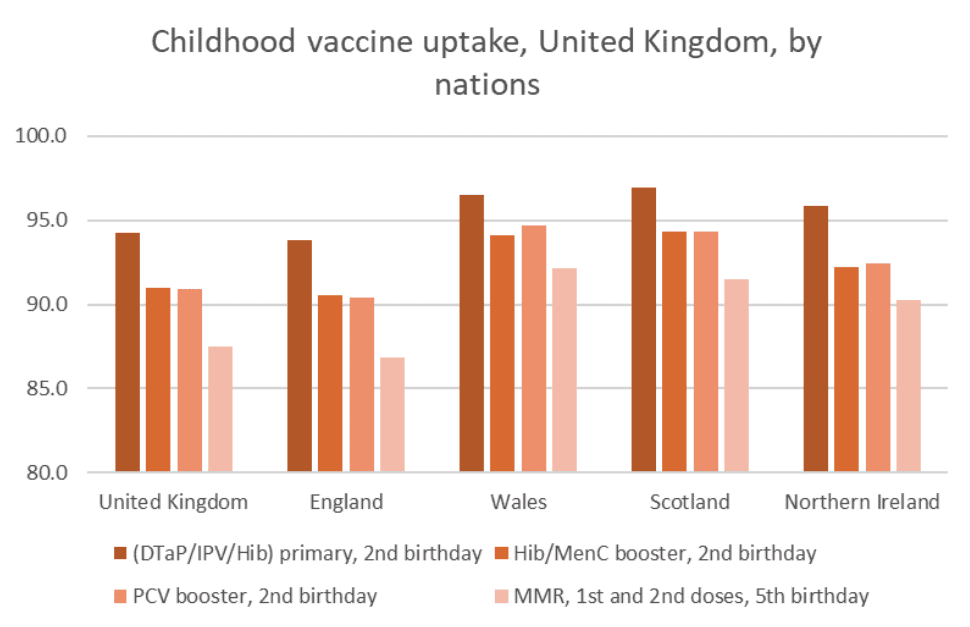
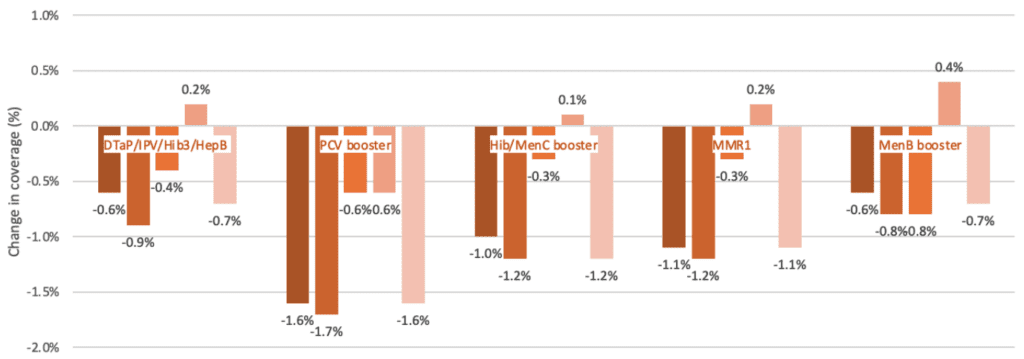
A similar approach is now required for immunisation policy in England. In the mid 1990s, the country was an international leader, boasting high uptake, effective delivery infrastructure and a strong pedigree in the identification, development, commercialisation and assessment of new vaccines. Yet coverage rates of the routine schedule which provides protection against fifteen vaccine-preventable infections, has been in decline. According to the latest figures from NHS England, no routine childhood vaccination met the 95% uptake target set by the World Health Organization. Our leadership position is under threat.1Emma Wilkinson, ‘All childhood vaccination uptake falls below 95% target in England’, Pulse, 29 September 2022 [link]
To reverse this trend, we must understand how we got here. Our research suggests that decline has been driven by several factors: some due to how the vaccine is delivered locally; others systemic, such as data reporting; and others circumstantial.
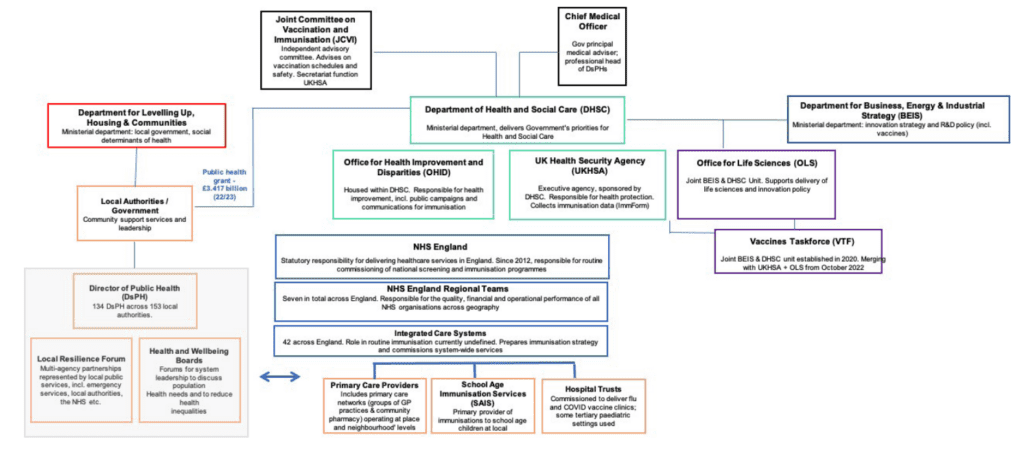
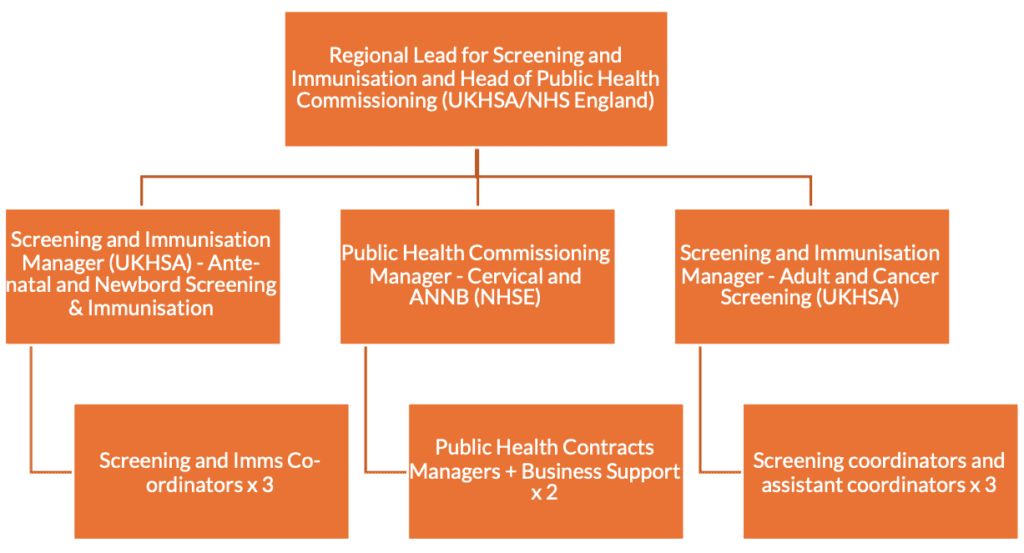
In chapter one we explore the policy context in detail. We have concluded that the governance and accountability arrangements for vaccination and immunisation are poorly understood and may themselves be contributory factors towards low uptake. Following the 2012 Health and Social Care Act, responsibility for vaccination was moved from primary care trusts (which were abolished) and instead held within a tripartite national delivery framework between NHS England, the Department of Health and Social Care, and Public Health England (whose responsibilities are now divided between UKHSA and OHID). Delivery is organised through a Local Operating Model. In the past decade, additional organisations have been introduced to the picture at a national level. Attempting to visualise interrelationships between these organisations as we have done in Fig. 1, page 30 is challenging.
In writing this paper we carefully evaluated the benefits that could derive from a streamlined structure. However, when set against the impact of disruption, we have concluded that it would be unwise to make major changes to the current tripartite arrangements. Vaccinations, as with other health protection initiatives, are complex and have multiple interfaces. Policymakers need to accept this. The focus should be on ensuring there is as much clarity as possible over decision making within the existing structure, rather than seeing reorganisation as the answer. We believe this is important to emphasise as a new Ministerial team joins DHSC, and NHS England moves towards a new operating model.
Clarifying responsibilities and communicating these externally would make a material difference. But more fundamentally it will need to be accompanied by an enduring political commitment to vaccines. Public health has been seen as a soft target for budget cuts when compared to the powerful interests within secondary care, where budgets have increased in real terms. By 2020/21, spending on the public health grant was 24% lower in real terms than it was during 2015/16. The Local Authority allocation for health protection work has been slightly better protected but was still 14% lower than five years earlier.2David Finch, Louise Marshall & Sabrina Bunbury, ‘Why greater investment in the public health grant should be a priority’, The Health Foundation, 5 October 2021 [link]
This misallocation of resource – away from prevention and towards medicalised healthcare – was unwise. Interventions to improve public health delivers phenomenal bang for buck: health protection interventions such as vaccines are calculated to deliver a £34 return for every £1 invested.3Rebecca Masters & Elspeth Anwar et al., ‘Return on investment of public health interventions: a systematic review’, Journal of Epidemiology & Community Health, Vol. 71, No. 8 (2017), 827-834 [link]
Health protection is an economic and a moral imperative. But it is also an area where the UK has pedigree, having been a world-leader in vaccine development, procurement, and delivery. The country’s rich history in discovery commenced with the smallpox vaccine, first tested by Edward Jenner in his Gloucestershire surgery, and culminated most recently in a licenced vaccine for COVID-19 based on technology designed by a team led by Dame Sarah Gilbert at the University of Oxford. Two world-changing public health discoveries – made 225 years apart, within 60 miles of each other.
Elements of the UK’s approach to the COVID-19 vaccine rollout were ‘world beating’, but many comparator countries have since outperformed the UK in uptake. The Vaccines Taskforce – heralded for its agility and overall effectiveness, is to become a joint DHSC and BEIS unit, meaning that competing priorities and processes may encumber its workings.4Sarah Newey, ‘Dame Kate Bingham: ‘Downing Street was indifferent about vaccines’, Daily Telegraph, 10 October 2022 [link] Now is the moment to take stock – to both ensure that immunisation targets are reached, and to ensure the UK is the best place to test and launch the next generation of vaccines.5For a useful, recent review of which considers the learnings from COVID-19 for routine programmes, see Kate Causey & Jonathan F. Mosser, ‘Learning from the COVID-19 pandemic to strengthen routine immunization systems’, PLOS Medicine, Vol. 19, No. 2 (2022), 1-18 [link] Whilst there has been a rhetorical rebalancing over the past two years towards the value of vaccination, coverage reports show that many of the routine immunisation programmes are experiencing slow catch up. Regression modelling and analysis undertaken for this report sets out the specific impact for measles and shingles – and are outlined in Chapter Two which considers the impact of the pandemic on immunisation.
In Chapter Three, we set out a vision for a new vaccination policy for England. Our vision is for an integrated delivery model with components at every level: national, system, place and across neighbourhoods. We are advocating in favour of greater autonomy for local teams to design campaigns in their patch, bringing together different assets locally but supported by a strengthened national data architecture and proportionate programme oversight.
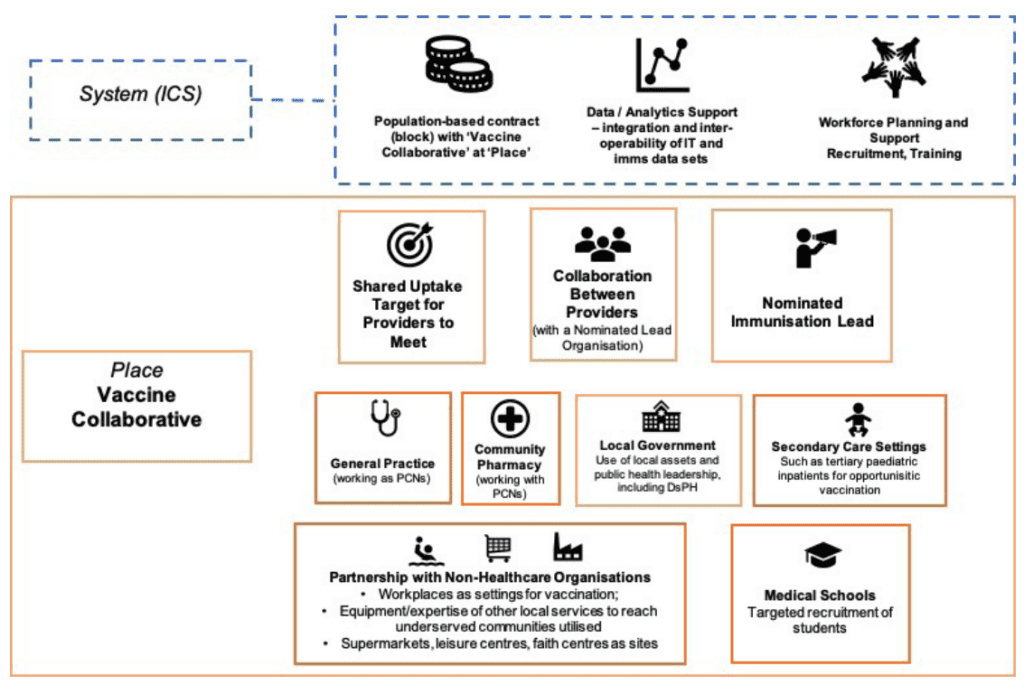
We know that being able to offer vaccination opportunistically is valuable, provided that data can be made available in the right places. So too is the trusted relationship between healthcare professional and patient in addressing legitimate doubts and wider hesitancy. Vaccinations – particularly those for children and of school age– should continue to be delivered within primary care or by School Aged Immunisation Services where the expertise and wraparound care of practice nurses, Immunisations Nurses, school nurses and GPs is a valuable asset. We want to see most resources tethered to that part of the system; but with a willingness to experiment with payment and provider models to allow community pharmacy to collaborate with colleagues in General Practice on a greater scale that we have seen in the past for adult programmes. The new Vaccination Collaboratives proposed in this report would allow deployment to be organised in a new way – shifting the accountability (and budget) onto local providers. A group of providers would be trusted to maximise their local assets to reach the highest possible coverage, with a particular emphasis on underserved groups. The tactics required to reach that target would be up for the local area to determine. In most instances, this could mean more of a role for local government, with the Directors of Public Health well placed to provide a leadership role. In others, we might see hospitals lean into their anchor institution role and become hubs for vaccination – such as those at high risk of being infected with influenza whose care may predominantly be in secondary care settings and where a dedicated clinic may be economical. We propose that these changes are piloted in three ICSs before wider national rollout.
This integrated model of delivery should become the default standard for rollouts, even in areas which do not enter into Vaccine Collaboratives. A single target could be introduced at neighbourhood levels to incentivise collaboration to reach the remaining 10-20% who are unvaccinated. Significantly, Policy Exchange believes there would be coherence to separate the planning of immunisations from screening services – currently delivered through a joint leadership team as part of Section 7A. Both would benefit from independent leadership and focus. Further details are outlined in Chapter Three.
Something we have heard clearly throughout this research is the strain on the healthcare workforce. There is a need to strengthen health protection capabilities across primary and community care more generally, but the current challenges necessitate tough choices. Having carefully considered the evidence, our view is that responsibility for adult vaccinations – particularly those of higher-volume, such as influenza and COVID-19, nurses, GPs and pharmacists should perform leadership and supervisory roles, with jabs delivered by a more heterogenous workforce. We recommend that the 35-40,000 medical students, 90,000 nursing students and 12,000 pharmacy students currently enrolled at universities in England are asked to volunteer to administer jabs for these two vaccines, being deployed each year to GP surgeries and community pharmacy during seasonal rollout campaigns, where they would support pharmacists, nurses and nursing assistants. These roles should be formalised.
We would expect a portion of the service to be seven-day and with extended hours enabled. This would be optimally planned at place level; with a minimum of one centre open per ICS footprint over weekends, resourced by the existing primary care community and the workforce groups mentioned above. The travel distances required for the public should be compensated by a well-resourced facility and smooth user experience.
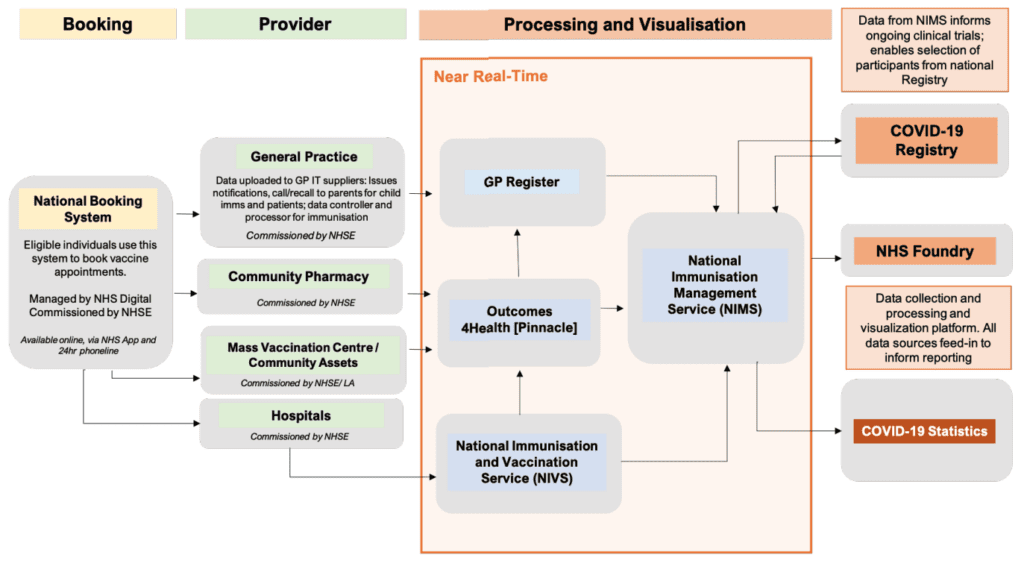
The integrated immunisation delivery model should commence with an improved offer for the service user. This should not mean a wholesale change. Vaccines – especially in infants and children – are wrapped up in cultural significance. Mucking around with where they are delivered and not recognising the expertise that the nursing profession in particular brings to this activity will cause confusion for parents and families and may lead to lower uptake. But that should not mean we should not try to make routine immunisations more accessible. The national booking service established for COVID-19 sets the expectation. Coupled with the existing approaches we believe this should allow for a high level of user experience, irrespective of background. Nearly 90% of the British population now owns a smartphone. Through the NHS App, citizens should be able to view their vaccination status across the routine schedule, upcoming appointments, and date of dose expiry. This is commonplace in other countries.
This will require changes from the public, who must become more engaged in their own health. Elements to expand health literacy can be driven through initiatives coordinated by the NHS and UK Government, such as encouraging further sign-up to a vaccination research registry (modelled on the successful COVID-19 Registry) or by adding functions to the NHS App. A nationwide press and media campaign may also be required – especially for future vaccines which may suffer from the ‘ripple effects’ of the pandemic, including vaccination fatigue or renewed challenges with vaccine confidence.
Beyond the organisations with statutory responsibility, there is a key role to be played by the VCSE sector and independent advocacy groups. No single organisation currently ‘owns’ the immunisation agenda, and vaccines can struggle for clarity of voice, particularly compared to well-mobilised patient advocates in cancer, cardiovascular, and metabolic diseases. Much like the prevention lobby, the pro-vaccine lobby is underpowered, with a dual mission of countering misinformation alongside conventional advocacy work to address legitimate hesitancy and reach underserved groups. A positive outcome of the pandemic should be the creation of a clearer standard bearer, independent of government, to champion immunisation across the life course.
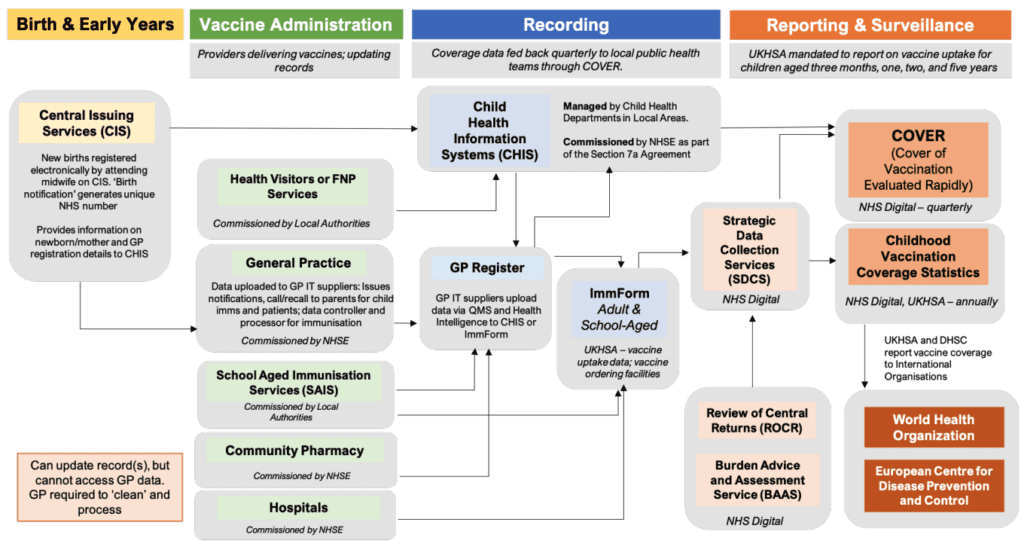
Effective data is the high-impact enabler of this new system. The aim should be for immunisation data to be accurate and seamlessly sharable across settings. In primary care, we need to move to a point where data is reliable and freely shared across pharmacy and general practice. This would be a transformation from the status quo. GPs have been wary of sharing patient data, often due to legitimate concerns.
The impasse on data sharing must be broken. Data can drive uptake itself, through planning deployment in a way as to maximise efficiency and reduce health disparities. Improved data quality will free up precious GP capacity, with too much time spent assessing national releases, affecting the quality of ‘call and recall.’ For secondary-use cases, data can provide an accurate helicopter assessment on vaccination performance across programmes, enabling appropriate and proportionate interventions to be made as a result. There is much to mimic from the approach to data recording and transparency during COVID-19 whilst realising that the unique circumstances during the pandemic which meant that good practice around co-design was sacrificed for speed. The Federated Data Platform creates an opportunity to build wide stakeholder support.
There is much to be excited about in vaccines. The pharmaceutical industry has developed a strong pipeline – in areas from Tuberculosis (which has not had a new vaccine in 100 years) to Respiratory Syncytial Virus (RSV).6‘Antibody jab approved for common winter virus RSV’, BBC News, 10 November 2022 [link] Whilst a lively discussion takes place regarding the wider prevention agenda, and a political focus on limiting the growth in the NHS budget to sustainable levels, this is an optimal moment to refresh current approaches to horizon scanning, modelling and health technology assessment. This should be accompanied by proportionate reforms to the Joint Committee on Vaccination and Immunisation (JCVI) to strengthen the transparency of its decision making. On the other side of the equation, manufacturers should engage in more active and early dialogue with governments and assessment bodies – echoing the ‘demand signalling’ mechanisms which have become commonplace in medicines. Outbreaks of monkeypox and re-emergence of polio in 2022 demonstrate that there can be no place for complacency.
This report makes 15 recommendations. Six are designated as critical recommendations which should be implemented immediately.
We are confident that, if implemented, this set of proposals would provide a strong basis for future vaccination policy. This will not only pave the way for new discoveries, following in the footsteps of Gilbert and Jenner. In some areas it will require a bold leap forward by policymakers, taking a calculated risk to get England’s coverage rates back into the gold medal position. But if these ideas make the boat go faster, what are we waiting for?
Next chapterOur Proposals in Brief
Six critical reccomendations – which we believe should be taken forward at the earliest opportunity – are highlighted in light orange
| Recommendation | Responsible Organisation(s) | Delivery Timescale | Implementation |
| National Leadership | |||
| 1.Enhanced Ministerial oversight through a new National Immunisation Board; clarify organisational remit and leadership roles for bodies responsible for health protection (incl. vaccination) (p .62) | No 10, DLUHC, DHSC, UKHSA, OHID, NHSE | By 2023 | The National Immunisation Board should meet for the first time in Q1 of 2023. Publish a National Vaccines Strategy by end of 2023. Where appropriate, the Board should meet, aligning with relevant groups in the devolved administrations such as the newly established Vaccination Delivery Board in Wales. |
| 2. Establish a National Immunisation Service (NIS) in England (p. 65) | NHS England, NHS SBS, NIHR, DHSC, DCMS | By 2024 | Define the scope and focus of NIS; establish a communications cell (aligned to Recommendation 13); enhance R&D capabilities (aligned to Recommendation 12). |
| 3. Separate immunisation from screening with distinct leadership and focus (evolutions to planning of Section 7A) (p. 67) | DHSC, NHSE, Local Government, SITs | By Autumn 2023 | Announce changes & issue advice by early 2023; implement changes by flu season in 2023, supported by the development of the NIS. |
| 4.Establish Vaccine Collaboratives in 3x pilot areas (p. 70) | NHS England, UKHSA, OHID, Local Government (incl. DsPHs), VCSE sector | By 2025 | Issue guidance and commissioning intention by 2023/24 with initial expressions of interest before assessment. First Vaccine Collaboratives to launch in 2024/25.
Requires amendments to GMS Statement of Financial Entitlements and the Community Pharmacy Contractual Framework to allow for capitated budget with automatic clawback mechanism. |
| 5. DHSC and DLUHC encourage ‘stocktakes’ from Health Protection Boards to understand localised under provision and inform best practice (p. 75) | DHSC, DLUHC, Local Government, NHS England, UKHSA | By 2024 | Health Protection Boards (chaired by the local Director of Public Health) should conduct a ‘stocktake’ of local vaccination efforts to inform National Vaccines Strategy by Autumn 2023. |
| 6. Delegate Immunisation delivery to ICBs to enable increase in ‘evergreen’ offers (p. 76) | DHSC, NHSE, ICSs, Local Government | By 2024 | Additional support for specialist clinics (such as for those with learning disabilities) where provision at greater scale is an advantage. |
| Workforce | |||
| 7. Make the health protection workforce a key plank of a longer-term workforce strategy (p. 81)
|
DHSC, NHS England, HEE, VCSE | 2023-2028 | Enable nursing, medical and pharmacy students to opt-in to deliver seasonal vaccination (p. 93); NHS England to formalise roles and introduce contracts, reimbursement arrangements and medical indemnity. Create routes for experienced GPs, nurses and pharmacists to re-enter the workforce, undertaking immunisation activities as a protected activity. |
| 8. Establish Neighbourhood Immunisation Coordinators (p. 81) | NHS England, Local Government | By 2024 | Conceived as part of the Integrated Neighbourhood Teams proposed by the Fuller Review
|
| 9. Adapt the National Protocol and National Patient Group Direction (PGD) mechanisms to maximise the vaccination workforce, where it can be done so safely (p. 81) | NHS England, Local Government, VCSE
|
By 2024
|
Clarify indemnity for non-clinical workforce; maintain national protocols, such as Regulation 2 of the NHS Regulations 2013; amend The Human Medicines Regulations 2012 to enable pharmacy technicians to administer vaccines under a PGD |
| Data | |||
| 10. Create a comprehensive immunisation information system (IIS) to modernise immunisation data collection and analysis (p. 86) | DHSC, NHS EngIand, UKHSA, MHRA, NIHR
|
2023-2028 | Integrate UKHSA surveillance systems as well as databases held by the MHRA and NIHR. A centrally-commissioned communication capability should also be introduced. Its specification should cover invitation, booking and preparation processes. This could be modelled on the current Covid-19 & Flu National Booking System to enable lead organisation in a ‘Vaccine Collaboratives’ to reach patients via the NHS App, SMS, email or phone. |
| 11. Enable both care provider and patient access to health records (p. 93) | DHSC, NHSE | 2023-2025 | Introduce joint controllership of patient data between GP practices and NHS England; add data breaches to Clinical Negligence Scheme for General Practice (CNSGP); enable community pharmacy (as a priority) to access patient records to support immunisation |
| Engaging Citizens | |||
| 12. Additional functionality within NHS App, incorporating the ‘digital red book’ and an NHS Research Registry (p. 103) | DHSC, NHSE, NIHR | By 2024 | Improvements to booking function incorporated as part of enhancements to NHS App; development of a comprehensive Vaccine Research Registry to drive user and life sciences sector engagement (p. 125) |
| 13. Development of a permanent comms cell in the NIS to tackle vaccine disinformation (p. 95) | DHSC, NHSE, DCMS | By 2024 | Model on Rapid Response Unit introduced by Cabinet Office during the COVID-19 pandemic. |
| 14. Establish an umbrella Life Course Immunisation advocacy group (p. 101) | VCSE | By 2024 | Establishment of new charitable organisation, drawing upon expertise and talents across VCSE sector. |
| Assessment and regulations | |||
| 15. Evolve the workings and processes of the JCVI (p. 105) | DHSC, UKHSA, JCVI | 2022-2025 | Establish a dedicated ‘Horizon Scanning Sub-Committee’; Update the JCVI Code of Practice. |
Next chapter
Policy Recommendations
National Leadership
- The Government should set out plans to clarify the national governance structures for immunisation. Vaccines policy in England should have clear ministerial oversight (with a single Minister covering all elements of health protection). Whilst improved coordination between bodies is essential, we do not recommend organisational reform. New organisations, including UKHSA and OHID require time to ‘settle’ and for responsibilities to be clarified.
- The Vaccines Minister should establish and chair a new National Immunisation Board – emulating the National Genomics Board. The remit of the board would be England-wide, complementing similar arrangements being established in Wales. Membership would include the tripartite, alongside representatives from provider organisations responsible for vaccine deployment (including local government and/or The Association of Directors of Public Health. External experts would be invited on an ad-hoc basis. The objective would be to create a platform for the Minister to scrutinise progress and to hold programmes to account, not to duplicate the role and function of the JCVI in giving independent advice nor existing forums for dialogue with manufacturers. The Board would meet (at least) once every six months.
- UKHSA should hire a Commercial Director to support ongoing work of the VTF and should focus future investment to enhance surveillance capabilities.
- Over time we would expect to see a consolidation of the role of the NHS England Regions, a redeployment of resource to ICSs and more shared policy work across NHS England and DHSC. This should be gradual rather than immediate given the importance of the catch-up programme and the detrimental short-term impacts that a restructure may create.
- DHSC should publish an overarching Vaccines Strategy. This should be refreshed every five years henceforth, taking a ‘life course’ approach, fulfilling a commitment set out in the 2020 Prevention Green Paper.7‘Closed consultation – Advancing our health: prevention in the 2020s’, Gov.uk, 22 July 2019 [link] The strategy should look to ensure that the most recent NICE guideline on improving vaccine uptake is adopted, universally.8Vaccine uptake in the general population, NICE guideline [NG218], 17 May 2022 [link] More broadly, our view is that the strategy should assume that responsibility for administration and deployment of most vaccines will remain in primary care and be led by general practice. There are two exceptions. A) The school-age immunisation schedule should continue to be delivered by SAIS providers in schools. B) For adult vaccinations we see an enhanced role for community pharmacy and the greater use of a ‘surge’ workforce capacity, with a formalised role for medical, nursing and pharmacy students in seasonal rollouts.
Delivery Models
- NHS England should establish a National Immunisation Service (NIS). NHSE should clarify at the earliest opportunity that the NIS would not represent a national delivery model for vaccines, but would represent a set of supportive services for ICSs, primary care providers and public health teams. All vaccinations across the life course should be incorporated within the work of the NIS (including COVID-19 and flu).9‘COVID-19 Vaccination Strategy for 2022 published’, Welsh Government, 24 February 2022 [link] Moreover, it should proceed on the basis of improved alignment between approaches taken across the devolved nations – in the future model, service users should be able to receive a first jab in England and a booster in Scotland, minimising fragmentation in service provision. This should be enabled despite devolved administrations developing their own delivery models (such as the ‘hub model’ being developed in Scotland). We believe it should focus upon strengthening the following elements at a national level:
- R&D capabilities, including working with NIHR to enhance patient registries and to support clinical research;
- Ensuring a consistent national voice on misinformation (with a dedicated communications cell working w/ DCMS and DHSC;
- Creating a more effective ‘pull system’ for providers and strengthening role of NHS Shared Business Services to cope with ‘surge’ demand and to support providers beyond secondary care;
- Simplifying mutual aid between providers.
We also believe the NIS can lock-in some of the positive consumer-focused initiatives developed during the pandemic. This should involve the creation of a national booking service across vaccination programmes – with the option to book, change, or cancel appointments at a range of settings (where applicable). The booking service for COVID-19 vaccines sets the minimum expectation.
- As part of the creation of a NIS, NHS England should re-examine how Section 7a responsibilities (commonly known as public health commissioning) are planned. Immunisation and screening programmes are currently combined under a single team within NHS England with leadership from a National Director. Our contention is that screening and immunisation are distinct from each other, and it will increasingly be necessary for them to be planned for separately, given both programmes grow in number and complexity. In reviewing the operationalisation of S7a, the Government and NHS England should review current gaps in provision – or where vaccination is recommended but isn’t covered by routine S7a programmes. An example would include a patient who has had a bone marrow transplant and require a full course of vaccinations. Community pharmacy should be commissioned to deliver all adult vaccinations through National Enhanced Services.
- NHS England should announce a pilot for the development of ‘Vaccination Collaboratives.’ The 2021/22 GP contract saw vaccination and immunisation become an essential service with a standardised item of service (IoS) fee set at £10.06 for most vaccines. A graded points system was introduced to incentivise surgeries to reach 95% coverage. These were the most significant reforms to immunisation payments in three decades, and need time to bed-in nationally. However, the broader shift within the system to new, non-activity payment methods should create opportunities for a collaborative approach on vaccination too. In the pilot area, the IoS payment would be replaced by a population-based contract to a ‘Vaccination Collaborative’ – bringing together community pharmacy, general practice, local government, the VCSE sector and other providers to collectively meet the needs of their citizens. We foresee a key role for local Directors of Public Health and the involvement of local authority commissioned health outreach and inclusion teams. This approach could take the form of a pilot amongst three ICSs (each representing a rural, semi-urban and urban demography). Amendments may be required to the GMS Statement of Financial Entitlements, and the Community Pharmacy Contractual Framework to allow for the novel payment mechanism. The principal objective would be to pool resources most efficiently, free up clinical time for other activity and improve uptake amongst underserved populations.
- DHSC and DLUHC should encourage Health Protection Boards (chaired by the Director of Public Health) to undertake local ‘stocktakes’ of vaccination uptake, to profile disparities and to analyse efforts required to better meet the needs of underserved communities by Autumn 2023. NHS England and OHID should collate and publish combined best practice guidance for vaccination services. Whilst there is no shortage of best practice, this is not currently compiled and published nationally. This exercise should draw upon evidence from CQC, the most recent NICE guideline, system level coverage reports as well as integrating the work of the London School of Hygiene & Tropical Medicine’s Vaccine Confidence Project. Most significantly it should highlight the processes and steps taken to achieve the outcome, emphasising repeatability.
- The commissioning of immunisation should be delegated to integrated care boards (ICBs) over time to strengthen whole-system approaches to health protection. The new ICS structures should play a role in enabling an ‘evergreen’ immunisation offer at a local level, both commissioning and providing oversight to traditional providers and Vaccine Collaboratives where they are established. Expertise for vaccination currently sat within the NHS England Regions is valuable and should be gradually redeployed to ICSs as NHS England Regions take on a more strategic role. Within this:
- ICBs should commission ‘evergreen’ immunisation offers to support those from traditional providers, including mobile and pop-up vaccination units (such as vaccination buses) to target outreach of underserved groups, such as the homeless, in popular locations, such as supermarket car parks and town centres.
- Additional support should be provided to ensure improved provision of ‘specialist’ vaccination clinics to improve uptake amongst those with learning disabilities and autism. There are roughly 30,000 people with learning disabilities within each of the 42 ICS footprints. A specialist clinic would typically involve relatively minor adaptations to an existing site to make it a calmer environment, with longer, staggered appointments and a higher proportion of staff with relevant expertise, such as learning disability nurses.
- Neighbourhood immunisation coordinators should be created [see recommendation 11]
- ICSs should consider the possible benefits of non-traditional providers boosting their immunisation offers. Children’s hospitals and units with emergency and tertiary paediatrics have potential to deliver childhood immunisations, although this must be carefully modelled to determine whether the return is justified given the additional requirements, including enabling data sharing from Child Health Information Services (CHISs). Examples which could prove beneficial across the adult programme would include specialist HIV clinics.
Workforce
- The immunisation workforce should be rethought as part of the new fifteen-year workforce strategy being developed by the Government. Most vaccines are delivered by practice nurses, school nurses, immunisations nurses, community pharmacists and GPs. This workforce – operating primarily across primary and community care should be strengthened and expanded, recognising the benefits to having a workforce with specific expertise in immunisation. In addition to the role played by Health Education England, there will be a critical role for the Local Government Association and The Association of Directors of Public Health in informing strategic workforce planning for health protection. We see significant opportunities for training and workforce planning to be streamlined and strengthened as a consequence of the merger of NHS England and Health Education England.
- Efforts to leverage the attractiveness of vaccination activity should encourage the development of dedicated schemes at system level, to enable recent retiree healthcare professionals, including nurses, GPs and pharmacists to undertake vaccination work as a specific, and protected activity.
- All medical, nursing and pharmacy students should be able to opt in and trained to deliver immunisations – except where there is a strong clinical rationale for not doing so (or adequate supervision cannot be assured). A new minimum expectation will encourage students to support with vaccine deployments for at least two days over the course of their studies. This approach should be formalised, with contracting and reimbursement for sessions delivered introduced.
- A greater role for volunteers, enlisted to work within a dedicated local footprint – either as part of a Vaccine Collaborative or other primary care provider during surge periods (particularly the seasonal rollouts of influenza and COVID-19 vaccines). This would seek to take advantage of the existing trained volunteer workforce (St John Ambulance trained 26,500 volunteers during the pandemic.) This approach should explicitly draw on recently trained volunteers – some of whom developed the capability to train members of the public to vaccinate.
- The creation of new pathways for non-clinical staff and volunteers to develop skills and experience – so that some can become specialist immunisers with further training. Encouraging uptake of Royal Society for Public Health qualifications should be encouraged by systems, whilst NHS England should clarify medical indemnity for the non-clinical workforce.
- Neighbourhood Immunisation Coordinators should be established as part of the ‘Integrated Neighbourhood Teams’ proposed by the Fuller Review. These would be named individuals who can respond to queries and provide a local focal point. The role would typically be filled by a clinician or public health expert although that is not a requirement. It would be the equivalent of 0.25 whole time equivalent role, paid at AfC band 8a. Concurrent with most the recent NICE guideline, this could overlap with the nominated person responsible for identifying housebound immunisers.
- Adapt the National Protocol and National Patient Group Direction (PGD) mechanisms to maximise the vaccination workforce, where it can be done so safely. This would include:
- Adding Pharmacy Technicians to those able deliver vaccines through a Patient Group Directive (PGD) with an amendment to The Human Medicines Regulations 2012. It would be important however to ensure that any changes are accompanied by strengthened quality assurance measures.
- Proportionate amendments to the National Protocol, such as adapting Regulation 2 of the NHS (Performers Lists) Regulations 2013 (which removed the requirement for those administering COVID vaccine to be registered on the medical performers list) should be maintained where it is clinically appropriate to do so.
Data
- DHSC and NHS England should create a comprehensive immunisation information system (IIS) to modernise immunisation data collection and analysis, drawing upon international best practice, so that everyone works from a ‘single version of the truth.’ (CRITICAL RECOMMENDATION). This should involve the following changes:
- Creation of a single national platform. Following the successes of NHS Foundry as part of COVID-19 vaccine deployment, the NHS is currently tendering for a Federated Data Platform (FDP), in a multi-year deal worth up to £360m. Vaccination and immunisation is included within five indicative use cases. We believe that the FDP should – at a minimum – offer the ability to integrate with existing GP patient records, to allow for population cohorts and vaccine coverage reporting. Over time this ‘single version of the truth’ should be used (with varying levels of access) across the health and care system. Coverage reports should be broken down by neighbourhood, place, and system.
- Within an ICS level, each system should appoint data managers to oversee data quality within the FDP.
- A centrally commissioned communication capability should be introduced alongside this. Modelled upon the current Covid-19 and Influenza National Booking System, the aim is to enable providers (and eventually, ‘Vaccine Collaboratives’) to choose software from a nationally specified framework which would cover invitation, booking and preparation processes. The framework should specify that cover a variety of channels, including NHS App, SMS, email and telephone.
- NHS England should enable all patients and relevant healthcare professionals’ access to their immunisation records to enable ‘opportunistic vaccination’. We also propose joint controllership over data between GP surgeries (who currently act as controllers and processors of data) and NHS England, to enable access for anonymised personal information for clearly defined purposes. As a priority, community pharmacy should be able to access patient records in order to support ‘opportunistic vaccination’ in the community. This move would also be a key component of a wider shift to ‘patient managed’ records, a move commensurate with commitments in the Government’s recent Plan for Digital Health and Care and the Integration White Paper, both of which call for the NHS App to offer a personalised experience and to encourage them to engage in tailored preventative activity (including immunisations and vaccinations).10A plan for digital health and social care, Department of Health and Social Care, 29 May 2022 [link]; Health and social care integration: joining up care for people, places and populations, Department of Health and Social Care, 9 February 2022 [link] The Vaccine Data Resolution Service (VDRS) should become more accessible to users so they can help to ensure records are up to date.
Engaging Citizens
- Additional functionality should be added to the NHS App – building on the commitment made by the previous Secretary of State for Health and Social Care which called for all COVID vaccinations to be bookable via the App by March 2023. The aim should be to ensure that service users (or relevant nominated persons) can access full ‘life course’ immunisation records, as well as having the ability to book and manage immunisation appointments.
- These developments should incorporate the existing work on developing a Digital ‘Red Book’ and embed the current ‘Birth to Five’ resource.11‘Digital revolution to bust COVID backlogs and deliver more tailored care for patients’, Gov.uk, 29 June 2022 [link] As part of an extended digital offer, e-Consent for childhood and school age immunisation should be offered to patients and carers wherever possible (and should accompany paper-based approaches in a longer-term transition to a predominantly digital approach). To mitigate digital exclusion, this information should be available via multiple channels, with paper-based resources remaining in place.
- Interest and user engagement in vaccines research should be strengthened by NHS England and the NIHR through the development of a comprehensive Vaccine Research Registry, modelled on the COVID-19 Vaccine Registry. Such an approach was genuinely world-leading during COVID-19 and ought to be expanded to support NHS partnerships with the life sciences sector.
- A coalition of charity and voluntary sector organisations should establish a Life Course Immunisation Advocacy group. This new organisation would provide information, act as the public champion and advocate for all immunisation programmes. This could emerge as a federation of existing Voluntary, Community and Social Enterprise (VCSE) organisations to ensure resources are pooled most effectively.
- Vaccine disinformation should be monitored and countered with the development of a permanent communications cell in the NIS, working closely with DHSC and feeding into the DCMS Counter Disinformation Unit. This should be modelled on the Rapid Response Unit introduced by the Cabinet Office during COVID-19 and should provide monitoring and asset creation to assist local providers tailor their own communication strategies and to deploy their own disinformation measures.
Assessment and Regulation
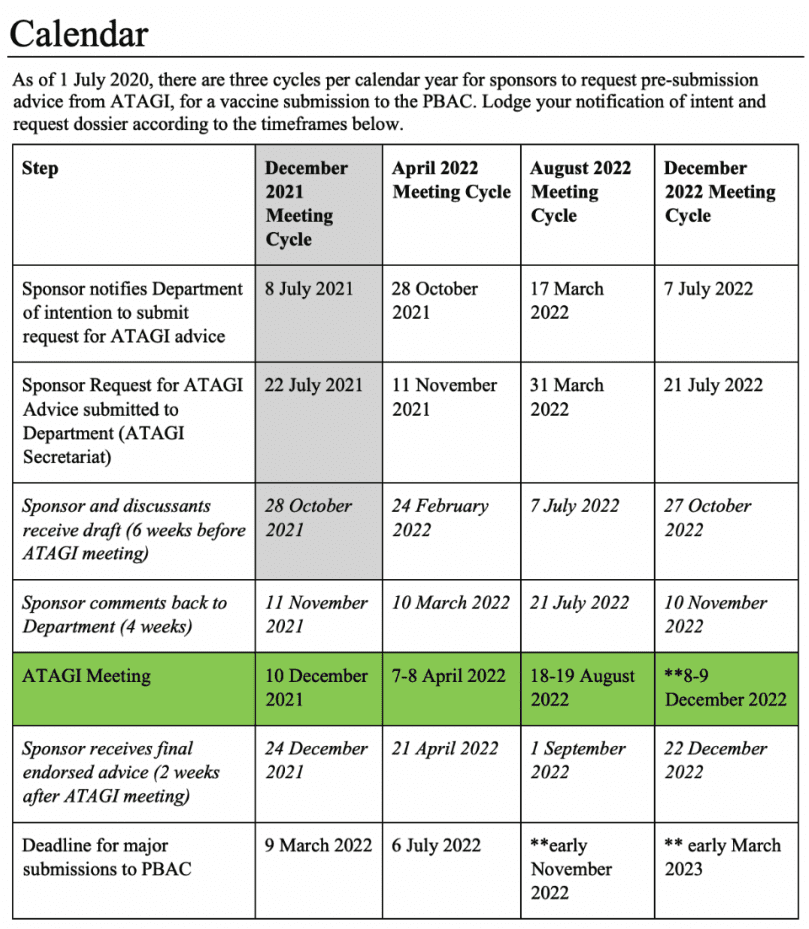
- Reforms should be introduced to modernise the approaches and workings of the Joint Committee on Vaccination and Immunisation (JCVI). These should be reflected in an updated JCVI Code of Practice. To support its world-leading work, the JCVI (and UKHSA) requires additional support. A busy ‘late stage’ vaccines pipeline means that demands placed upon it will be great in the coming years. Evolutionary changes to its workings should look to capture the positive learnings from the pandemic, by creating a stronger predictive arm, a more transparent decision and process architecture with the aim of enhancing dialogue with industry and key stakeholders, including NHS England. Changes would include:
- The establishment of a dedicated ‘Horizon Scanning Sub-Committee’, with a remit to look up to 10 years ahead (the current horizon scanning process looks at vaccines in development over the next 3-5 years). The sub-committee should be encouraged to ‘direct the horizon’ with demand signalling mechanisms which determine the nationally significant vaccine-preventable diseases. Representation on the sub-committee should include epidemiologists but may also draw upon the input of representatives from the Accelerated Access Collaborative, BEIS, DHSC and NHS England.
- An expansion of the opportunities for patient and public involvement.
- A refreshed approach to engagement with manufacturers, with routes created to allow for informal two-way dialogue to supplement company days.
- A clear timeline for the assessment of new vaccine candidates including a process chart which should be published on the JCVI website.
- Additional resource to ensure the JCVI can meet this expanded remit. As set out in the terms of reference, this should enable an expansion of the secretariat headcount, with emphasis on expertise in communications, horizon scanning and modelling.
Introduction
This report explores the future of vaccines policy in England. At a time when we are spending more on the NHS than ever before to meet increasing demand and growing complexity, immunisation remains the vanguard of preventative healthcare. Unlike other totemic public health issues such as obesity or smoking, there is a consensus both within Government and across mainstream political parties on the value of immunisation and the need to improve performance.
It would be legitimate to argue that routine vaccination should be afforded the same priority as waiting list backlogs, ambulance handovers, or appointments in general practice. Public health is connected to all these issues, and the value of vaccination for the NHS – and indeed the broader economy – is difficult to overstate. Whilst representing a cost to the taxpayer in the first instance, longer-term savings are derived through significant reductions in health costs and through the avoidance of productivity losses across the workforce.12Sachiko Ozawa & Samantha Clark et al., ‘Return on Investment from Childhood Immunization In Low- And Middle-Income Countries, 2011–20’, Health Affairs, Vol. 35, No. 2 (February 2016) [link] By Autumn last year, COVID jabs had – by the Government’s estimation – prevented over 100,000 deaths and at least 230,000 hospitalisations.13COVID-19 vaccine surveillance report published, Gov.uk, 14 May 2021 [link] That is before you consider the value routine immunisation programmes in their totality: of HPV vaccines in reducing incidences of cervical cancer; or Hepatitis B for cancers of the liver.14Till Bärnighausen & David E. Bloom et al., ‘Valuing vaccination’, Proceedings of the National Academy of Sciences, Vol. 111, No. 34 (2014), 12313-12319 [link] Success across the UK has ripple effects with effective immunisation playing an important role in reducing the global burden of disease.15 Immunization Agenda 2030: A Global Strategy to Leave No One Behind, World Health Organization [link]; Lawrence D. Frenkel, ‘The global burden of vaccine-preventable infectious diseases in children less than 5 years of age: Implications for COVID-19 vaccination. How can we do better?’, Allergy and Asthma Proceedings, Vol. 42, No. 5 (2021), 378-385 [link]
| ‘Vaccination’ or ‘immunisation’? |
‘Vaccination’ and ‘immunisation’ mean slightly different things, despite being used interchangeably in this report.
|
Declining performance
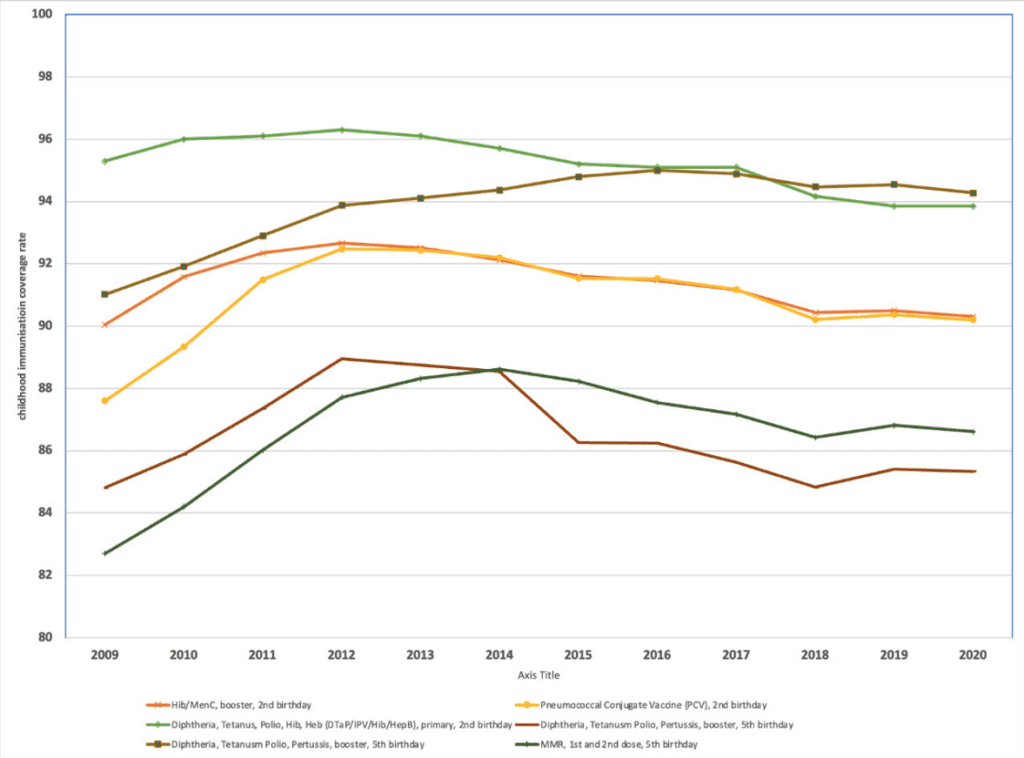
Graph 1. Childhood immunisation coverage, England, 2009/10-2020/21
Source: Childhood Vaccination Coverage Statistics, NHS Digital [link]
However, many routine programmes have witnessed declining uptake in recent years (see Graph1.). Within pre-school vaccinations, NHS England has missed every DHSC performance standard for uptake since 2012/13.16‘Investigation into pre-school vaccinations’, National Audit Office, 25 October 2019, p. 7 [link] In several instances, the picture of decline has been exacerbated by the pandemic.17Caitlin Tilley, ‘Decline in children receiving jabs for diseases other than Covid’, Pulse, 3 September 2021 [link] This aligns with a broader, global trend. For a comprehensive analysis, see Anita Shet, Kelly Carr & M Carolina Danovaro-Holliday, ‘Impact of the SARS-CoV-2 pandemic on routine immunisation services: evidence of disruption and recovery from 170 countries and territories’, The Lancet Global Health, Vol. 10, No. 2 (2022), 1-9 [link] and Kaja Abbas & Vittal Mogasale, ‘Disruptions to childhood immunisation due to the COVID-19 pandemic’, The Lancet, Vol. 398, No. 10299 (7 August 2021), 469-471 [link].
For evidence of disruption in a Canadian context for instance, see Hannah Sell, Ali Assi & S. Michelle Driedger et al., ‘Continuity of routine immunization programs in Canada during the COVID-19 pandemic’, Vaccine, Vol. 39, No. 39 (15 September 2021), 5532-5537 [link]. Programmes in Sweden maintained high levels of uptake however by comparison. See Kathy Falkenstein Hagander, Bernice Aronsson & Madelene Danielsson et al., ‘National Swedish survey showed that child health services and routine immunisation programmes were resilient during the early COVID-19 pandemic’, Acta Paediatrica, Vol. 110, No. 9 (June 2021), 2559–2566 [link]. MMR vaccine uptake has fallen to its lowest level for a decade, with coverage for the two doses in five-year-olds currently 85.5% (2020-21), well below the 95% World Health Organisation target needed to achieve and sustain measles elimination.18‘England: MMR vaccination awareness drive as uptake drops to lowest level in a decade’, Community Practitioner, 18 March 2022 [link] As Professor Helen Bedford and Helen Donovan have noted, this means that more than 1 in 10 children under the age of five are not fully protected from measles and are at risk of catching it.19Helen Bedford & Helen Donovan, ‘We need to act now to improve childhood vaccine uptake’, Institute of Health Visiting, 25 February 2022 [link] This led to the launch of a national campaign to remedy the situation in February 2022.20‘Around 1 in 10 children starting school at risk of measles’, Gov.uk, 1 February 2022 [link] Whilst there has been a shift in discourse around immunisations to encompass a ‘whole-of-life’ or ‘life course’ approach, coverage for some adult risk groups remains sub-optimal. The recent re-emergence of polio in sewage in East London (and the recommencement of a booster programme) as well as the recent outbreak of monkeypox reinforces the fragility of disease control and the need for a renewed approach.21Joe Pinkstone, ‘Polio vaccine will be offered to London children after virus found in sewers’, Daily Telegraph, 10 August 2022 [link]; Daniel M. Davis, ‘A little more vaccination: Elvis Presley and the race to beat polio’, The Times, 26 June 2022 [link]. Accordingly, recent JCVI minutes published on 5th August 2022 made a recommendation to move MMR2 to 18 months in order to increase VCRs and prevent potential outbreaks [link]
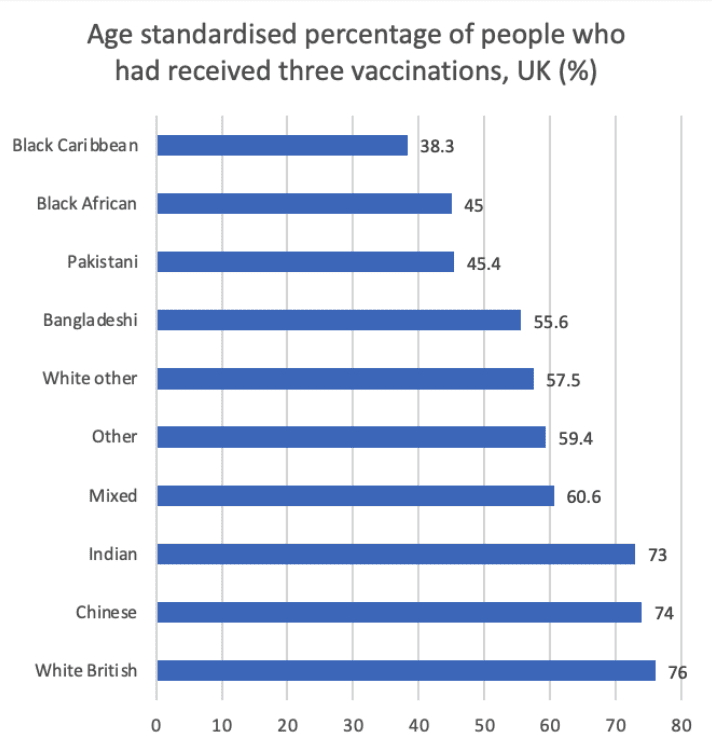
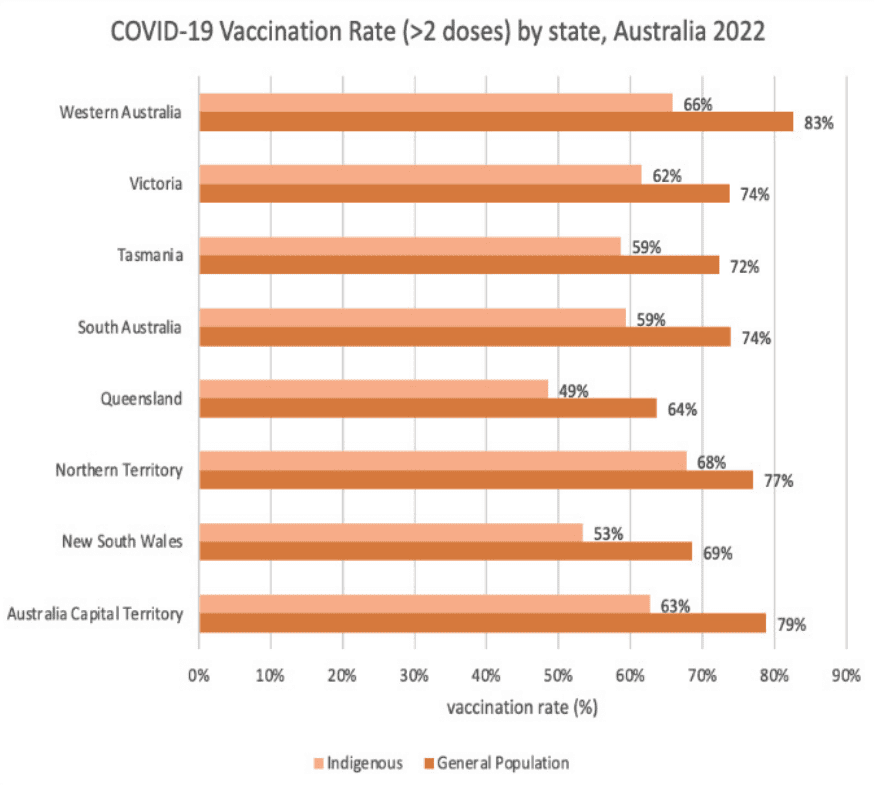
The general trend has been a decline in uptake across routine programmes, but this picture is varied across the country.22Investigation into pre-school vaccinations, National Audit Office, 25 October 2019 [link] Whilst there are long-standing challenges in London, despite early concerns, infant and preschool immunisation uptake increased in Scotland over the lockdown period.23Fiona McQuaid, Rachel Mulholland & Yuma Sangpang Rai et al., ‘Uptake of infant and preschool immunisations in Scotland and England during the COVID-19 pandemic: An observational study of routinely collected data’, PLoS Medicine, Vol. 19, No. 2 (February 2022), 1-18 [link] The current data also suggests there are particularly low levels of uptake amongst certain geographic, socioeconomic, ethnic and religious groups across England; many of whose healthcare needs are underserved more broadly.
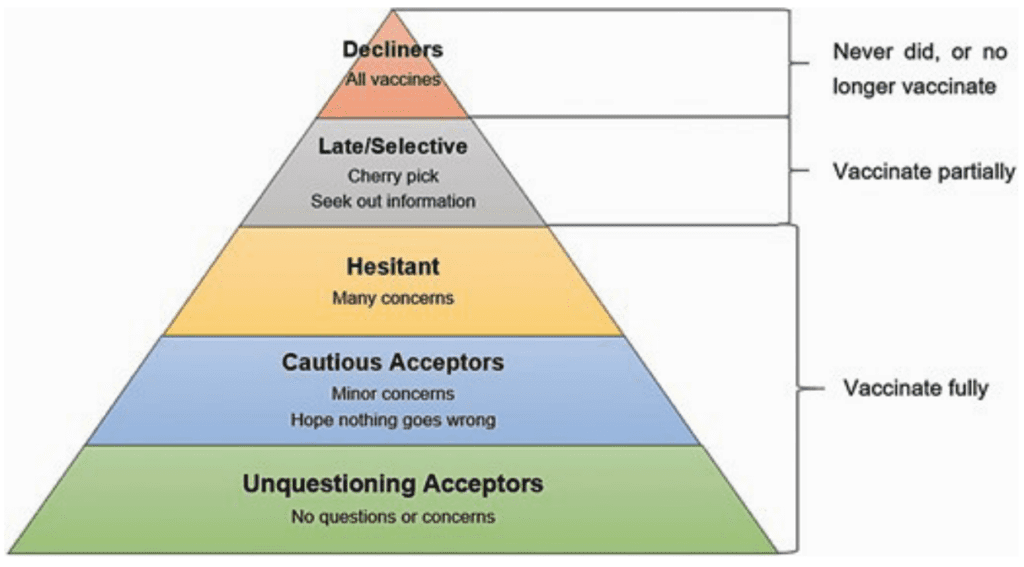
Whilst an overall trend in declining uptake is clear to see, what is less easily quantified are wider trends in vaccine confidence. Many healthcare professionals report confidence issues affecting uptake across childhood programmes, or ‘vaccine fatigue’ setting in. This necessitates a focus on baking in best practice undertaken by local government, PCNs and individual GP practices in reaching underserved communities and in effectively tailoring campaigns to meet need.
A renewed focus
The experience of the pandemic has encouraged a fresh look at immunisation services in the round. As England enters a new phase of our response to the pandemic, it is expected that the deployment of the COVID-19 vaccine will be folded into the current schedule.24COVID-19 autumn booster and flu vaccine programme expansion, NHS England, 15 July 2022 [link] This presents an opportunity to bring key learnings and to replicate them across the routine programmes, where applicable.
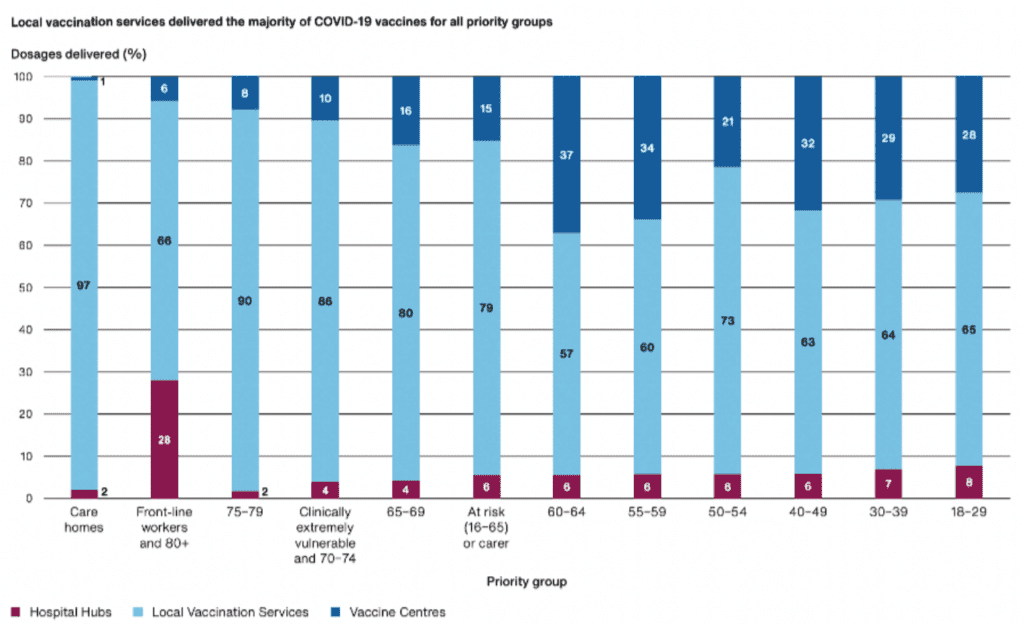
The factors that enabled a successful immunisation campaign are clear to see: focused and clear leadership; a sense of mission and speedy decision-making; supply chain resilience; workforce preparedness; localised strategies to target underserved communities.25Nicholas Timmins & Beccy Baird, The Covid-19 vaccination programme: Trials, tribulations and successes, The King’s Fund, January 2022 [link] A spotlight was also shone upon the world leading characteristics of the UK’s life sciences and healthcare sector. The Vaccines Taskforce (VTF) acted ‘decisively and cost-effectively’.26Government’s Vaccines Taskforce has worked “decisively” and at “great pace” to improve UK’s pandemic preparedness, Gov.uk, 8 December 2020 [link]; For a review of the VTF, see UK Vaccine Taskforce 2020 Achievements and Future Strategy: End of year report (December 2020) [link]. The VTF will shortly be merged UK Health Security Agency and the Office for Life Sciences, see ‘Vaccine Taskforce to merge with UKHSA and OLS’, Gov.uk, 15 June 2022 [link] The pandemic also encouraged innovation, much of which would not have occurred at the equivalent pace in ‘peacetime.’ From novel approaches to enable easier, granular data sharing (Control of Patient Information, or COPI), to arrangements to enable primary care providers to delivery vaccines in novel settings, such as supermarket car parks or large workplaces, the best of these initiatives should be replicated – where suitable – across other programmes. But ‘initiative decay’ is a real risk.27Datapwa Mujong, ‘Will reached communities become ‘hard to reach’ again?’, British Journal of General Practice, Vol. 71, no. 713 (2021) [link] Where engagement with underserved communities for instance was short-term and limited to COVID-19 vaccine deployment, fatigue and mistrust may arise in the future. The pandemic also represented a paradox with some disciplines experiencing a high level of command and control, whereas others were liberated from reporting requirements and encouraged to innovate in ways to better suit their local circumstances. As we learn to live with COVID-19, we need to find a new way of liberating and empowering those on the front line. This must be done in a sustainable way and should include strengthened national enablers in key areas such as data, workforce planning and resourcing.
There has been a sense for a number of years that the architecture of immunisation could be improved. Different Government departments and arm’s length bodies are responsible for elements of procurement, development and delivery (See Figure 1). Moreover, whilst ICSs have now been placed upon a statutory footing, questions remain as to how the work of Regional teams, primary care providers and local authorities will link with that of ICSs; whilst the VTF was heralded as a major success in tackling the pandemic, representing particularly strong performance in the procurement of vaccines and in engagement with manufacturers, there is a risk that folding the body into a joint UKHSA-OLS body may reduce its and agility – two features which underpinned its early success.28Government’s Vaccines Taskforce has worked “decisively” and at “great pace” to improve UK’s pandemic preparedness, Gov.uk, 8 December 2020 [link] As its former head has recently stated, there is a risk that the organisation takes its “foot off the gas” in finding innovative new ways to prevent the spread of Covid-19.29Jim Dunton, ‘Kate Bingham warns officials have ‘lost focus’ on new Covid jabs’, Civil Service World, 31 August 2022 [link]
Figure 1 – Current governance architecture for vaccines and immunisation in England
In January 2022, the former Secretary of State for Health and Social Care mooted the introduction of a ‘National Immunisation Service’. Work has now begun within NHS England to develop an ‘integrated vaccination and immunisation strategy’.30Letter from Steve Russell and Nikki Kanani to ICB Chief Executive Designates, NHS England, 22 June 2022 [link] The objectives are to reduce disparities in uptake by making vaccination more convenient and accessible, and to reduce the impact of vaccine deployments on ‘core’ GP services. There is a real possibility of quite substantial changes to the way in which vaccines policy is developed and how campaigns are organised as a result, depending upon how this work proceeds.
In that context, this report considers the future of routine vaccines delivered across the life course, assessing the impact of the slow catch-up over the course of the COVID-19 pandemic upon routine programmes, before setting out a series of proposals to improve coverage and to provide an improved service for users.31Tim Crocker-Buque & Sandra Mounier-Jack, ‘Vaccination in England: a review of why business as usual is not enough to maintain coverage’, BMC Public Health, Vol. 18, No. 1351 (2018) [link]
The structure of the report is as follows:
- Chapter 1 – Explores the historical and current immunisation policy context. It assesses the value of vaccination, through an analysis of the impact of reductions to the uptake of MMR and shingles vaccines during the early stages of the pandemic.
- Chapter 2 – Provides our assessment of the impact of the COVID-19 pandemic upon vaccines policy
- Chapter 3 – Sets out our vision for the design of vaccination and immunisation services in England, bringing together the key insights and findings from our research. This covers off the following core thematic elements of the programmes:
- Governance and Delivery Models
- Workforce
- Data
- Engaging Citizens
- Assessment and Regulation
- Conclusions
Methodology
We collected insights and tested our findings through semi-structured interviews with over 40 immunisation experts, policymakers, industry representatives, and international organisations between May and October 2022. These interviews included experts from Belgium, Portugal, and Australia to learn from innovative approaches to increase immunisation uptake internationally, as well as to learn from their experiences in horizon scanning and the evaluation of novel vaccine technologies. We also carried out two roundtables in May and June: one focused on the experiences within England; the other on international best practice respectively. We complemented these interviews and roundtables with a comprehensive literature review.
As part of this work, we have also undertaken a quantitative analysis of publicly available data to estimate the potential public health impact (in terms of case reductions and mortality) of increased uptake of MMR and shingles vaccines. These two programmes were chosen to represent impacts across the life course, given they are targeted at different demographic groups (childhood and adult).
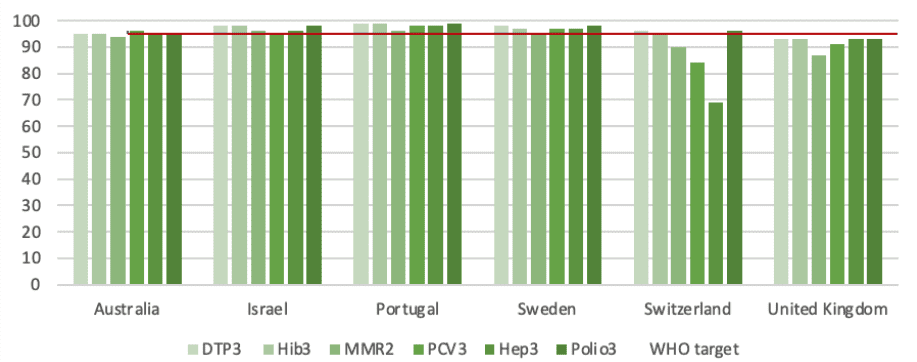
In each section of this report, we also look at international immunisation approaches taken in five different countries that have achieved high routine childhood vaccination rates (See Graph 2.) These include Australia, Israel, Portugal, Sweden, and Switzerland. We understand that each of the selected health systems are highly diverse in their organisational structures, operations, and political and economic characteristics. We do not therefore attempt to compare nor benchmark the performance of these countries but to draw upon insights from these high-performing healthcare systems.
Graph 2. Childhood immunisation uptake across five comparator countries
UNICEF (2019) [link]
Next chapterChapter 1 – Policy Context
In this chapter, we consider the structure of immunisation programmes in England and their development over time. We also explore the extent to which COVID-19 exacerbated the decline in uptake across routine programmes using Shingles and Measles coverage data as case studies to evaluate the number of cases that can be prevented annually if coverage were to achieve the WHO target of 95%.
England’s Immunisation Programme
Immunisation is widely considered as one of the greatest global health achievements in history––the WHO estimates that vaccines save 4-5 million lives per year.32Xiang Li, Christinah Mukandavire & Zulma M Cucunubá et al., ‘Estimating the health impact of vaccination against ten pathogens in 98 low-income and middle-income countries from 2000 to 2030: a modelling study’, The Lancet, Vol. 397, No. 10272 (2021), 398-408 [link] Immunisation is not only an extremely effective public health measure – with most vaccines producing immunity in over 90% of those vaccinated – but also cost-effective, benefitting not only those with direct protection, but others in their families and communities.
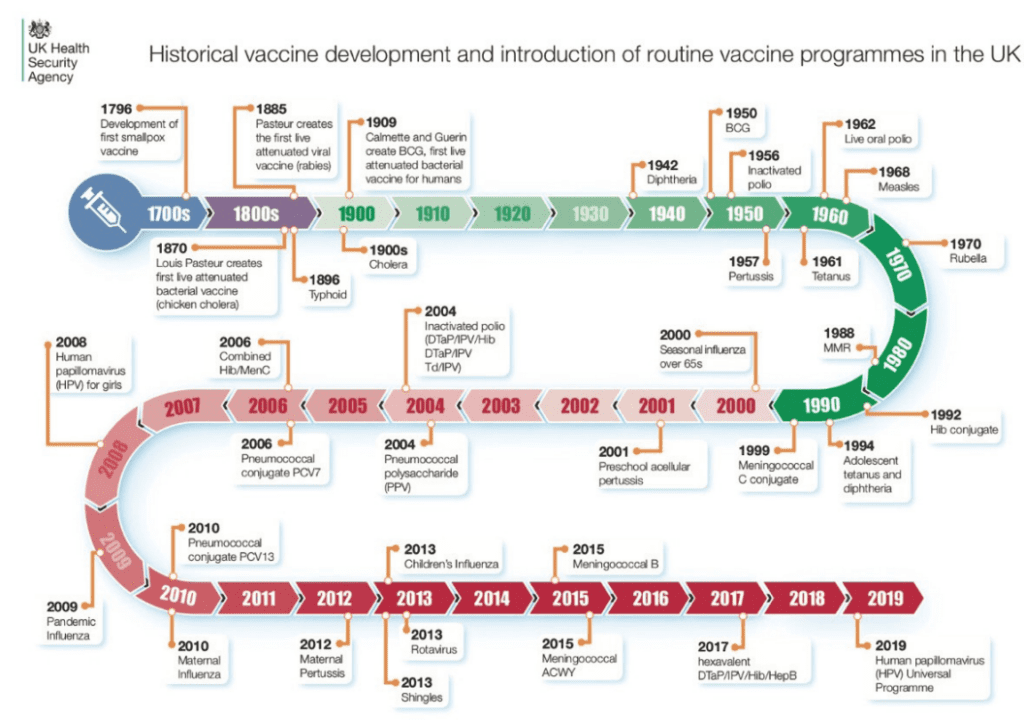
Life-threatening diseases such as diphtheria, whooping cough and polio used to be highly prevalent in children in the UK and are now extremely rare. In 1942, there were 50,804 diphtheria cases in England and Wales; now there is just one case a year on average (although its recent discovery at Manston asylum centre in November 2022 is a current cause of concern).33‘Manston asylum centre death may have been caused by diphtheria’, The Guardian, 26 November 2022 [link] There were 92,407 cases of whooping cough per year in 1957; now the incidence per year is 3,506. A recent study published in The Lancet has found that the HPV immunisation programme has almost eliminated cervical cancer in women born since September 1995.34Milena Falcaro, Alejandra Castañon & Busani Ndlela et al., ‘The effects of the national HPV vaccination programme in England, UK, on cervical cancer and grade 3 cervical intraepithelial neoplasia incidence: a register-based observational study’, The Lancet, Vol. 398, No. 10316 (2021), 2084-2092 [link] Figure 2 depicts the steady increase in vaccines which have been added to the routine schedule over time.
These interventions are significant in supporting population health and ensuring health systems are not placed under greater stress domestically, but the benefits of vaccination stretch far beyond healthcare spending to include wider economic, educational and health security benefits.35Peter Piot, Heidi J. Larson & Katherine L. O’Brien et al., ‘Immunization: vital progress, unfinished agenda’, Nature, Vol. 575, 119–129 (2019) [link] One study found that health protection interventions such as vaccines deliver a £34 return for every £1 invested.36Rebecca Masters, Elspeth Anwar & Brendan Collins et al., ‘Return on investment of public health interventions: a systematic review’, Journal of Epidemiology & Community Health, Vol. 71, No. 8 (2017), 827-834 [link]
Currently, sixteen vaccines and immunisations are offered on the NHS across the ‘life course’ (see Table 1). These are all ‘preventative’ vaccines, predominantly administered to healthy individuals. With Covid-19 vaccinations to be incorporated into routine immunisation programme in Wales, it is likely that a similar approach will be adopted in England in due course.37Emma Wilkinson, ‘Covid vaccinations to be incorporated into routine immunisation programme in Wales’, Pulse, 24 February 2022 [link] New vaccines in the pipeline are assessed and advise upon their use determined by the Joint Committee on Vaccination and Immunisation (JCVI), an independent expert advisory committee. Its role is discussed in further detail in Chapter 3.
Figure 2. Vaccination Timeline from the 1700s to present day
Source: ’Vaccination timeline infographic from 1796 to present’, UK Health Security Agency [link]
Table 1. Complete Routine Immunisation Schedule: Childhood, Adolescent, and Adult Programmes Delivered by the NHS in England
| Vaccine | When is it offered? | Where is it offered? |
| Babies under 1 year old | ||
| 6-in-1 vaccine (DTaP/IPV/Hib) | 8 weeks | GP surgery; local child health clinic
|
| Rotavirus vaccine | ||
| MenB | ||
| 6-1 vaccine (2nd dose) | 12 weeks | GP surgery; local child health clinic
|
| Pneumococcal (PCV) vaccine | ||
| Rotavirus vaccine (2nd dose) | ||
| 6-1 vaccine (3rd dose) | 16 weeks | GP surgery; local child health clinic |
| MenB (2nd dose) | ||
| Children and Adolescents 1 to 15 | ||
| Hib/MenC (1st dose) being discontinued | 1 year | GP surgery; local child health clinic
|
| MMR (1st dose) | ||
| PCV (2nd dose) | ||
| MenB (3rd dose) | ||
| Seasonal flu vaccine (Influenza) (every year) | Eligible age groups | GP surgery (6 months to primary school), School (primary school, year 7-11), Community clinic (home-schooled children) |
| MMR (2nd dose) | 3 years and 4 months | GP surgery; local child health clinic |
| 4-in-1 pre-school booster (DTaP/IPV) | ||
| COVID-19 vaccine (1st and 2nd dose) | 5 to 15 years
|
GP surgery, vaccination centre, pharmacy, walk-in vaccination sites (without appointment), school |
| HPV | 12 to 13 years | GP surgery, school |
| 3-in-1 teenage booster (Td/IPV) | 14 years | Secondary school |
| MenACWY | ||
| Adult | ||
| COVID-19 vaccine (1st, 2nd and booster) | 16 years and over | GP surgery, vaccination centre, pharmacy, walk-in vaccination centre |
| Flu vaccine | 50 years (and every year after)38It remains undecided (at the time of writing) whether the 65+ cohort will be lowered for 2022-23 to include 50-64 years (this may need to be updated to 65 years and every year after as a result). | GP surgery, pharmacy |
| Pneumococcal (PPV) vaccine | 65 years | GP surgery, pharmacy |
| Shingles vaccine | 70 years | GP surgery, pharmacy |
| Pregnant Women | ||
| Flu vaccine | During flu season | GP surgery, pharmacy |
| Whooping cough (pertussis) vaccine | From 16 weeks pregnant | GP surgery, antenatal clinics |
Source: The complete routine immunisation schedule from February 2022, NHS England [link]
In England, the coordination of immunisation programmes involves a wide range of organisations, and consequently, as one recent study describes it, the system is “a complex mesh”39Tracey Chantler, Saumu Lwembe & Vanessa Saliba et al., “It’s a complex mesh”- how large-scale health system reorganisation affected the delivery of the immunisation programme in England: a qualitative study’, BMC Health Services Research, Vol. 16, No. 489 (2016) [link]. The national strategy and performance targets are set by DHSC with advice from the independent JCVI and the Commission on Human Medicines (CHM); programmes are commissioned by NHS England; procurement and surveillance is undertaken by the UK Health Security Agency (UKHSA), forming a tripartite organisational structure that relies on ’joint responsibility.’ DHSC does not itself deliver vaccination programmes. Under the NHS Public Health Functions Agreement (Section 7A), DHSC delegates responsibility for delivering national immunisation programmes to NHS England. The latter then commissions vaccination services to GP surgeries, School Age Immunisation Services (SAIS), or community pharmacy, depending on the target population. Pre-school and adult vaccinations are usually delivered by GPs surgeries, commissioned through the GP contract. School-age services are commissioned by seven Regional NHS England teams, delivered through SAIS. Coordinating a national immunisation programme that serves a large and diverse population of 56 million is not an easy task, and as our report will explain, England’s immunisation programme suffers from fragmentation as a result.
Across the UK, immunisation programmes – as with the rest of health services – are devolved. This report focuses upon England’s experience, but Box 1 provides a summary of how programmes across the four devolved nations have recently differed.
| Box 1. Immunisation Programmes Across the UK | |||||||||||||||||||||||||
| How do immunisation programmes differ across the UK?
Prior to political devolution in 1999, the administration of each health service in Scotland, Wales and Northern Ireland was the responsibility of the respective Secretary of State.30 However, the convention of collective responsibility of the Cabinet potentially limited the Secretary of State for Scotland, Northern Ireland, and Wales to pursue policies that diverged from those applying to England. Table 2 illustrates the different organisations responsible for immunisation programmes across the UK. Table 1. Overview of organisations involved in immunisation across nations
Scotland: The Vaccination Transformation Programme (VTP) Whilst the majority of programmes were administered through general practice, in 2017, the Scottish Government and the Scottish General Practitioners Committee (SGPC) agreed vaccinations would move away from GP-based delivery to one based on NHS Board/Health and Social Care Partnership (HSCP) delivery through dedicated teams (as part of an effort to reduce GP workload)40Vaccination Transformation Programme, Public Health Scotland [link] |
|||||||||||||||||||||||||
| Wales
The Department of Health and Social Services in Wales sets expectations for NHS Wales to deliver and commission routine immunisation programmes, provided as nationally contracted services. The call/recall system is centralised, using a national birth registration-based system that generates named postal invitations sent to home addresses. 41Richard J. Roberts, Anne McGowan, and Simon Cottrell, ‘Measuring inequalities in immunization in Wales and the impact of interventions’, Human Vaccines & Immunotherapeutics, Vol. 12, No. 10 (2016), 2704–2706 [link] In October 2022, a National Immunisation Framework for Wales was published.42National Immunisation Framework for Wales, Welsh Government (October 2022) [link] Northern Ireland Immunisation policy in Northern Ireland is planned by the Department of Health (Northern Ireland), commissioned jointly by the Public Health Agency (PHA) and Health and Social Care Board and predominantly delivered through GPs and schools. It has a more centralised approach to the English system whereby the PHA is responsible for both the commissioning and surveillance of national vaccine programmes. |
|||||||||||||||||||||||||
| Summary
England currently has the lowest childhood immunisation rates across the UK (See Graph 3 below). In 2019/20, all nations apart from England reached the WHO target of 95% in DtaP/IPV/Hib coverage. However, overall routine childhood immunisation coverage has been in decline since 2013/14. For instance, immunisation for DTap/IPV/Hib peaked at 98.2% and 98.6% in Scotland and Northern Ireland in 2013/14; both have now dropped below 97%. The coverage of MMR first dose (by 5th birthday) peaked at 95.3% in 2016 and has been declining since. Routine childhood programmes were in decline across the UK before the COVID-19 pandemic, which further impacted on immunisation uptake (Scotland has proven the exception). Whilst each devolved administration has considered the development of a form of national immunisation service, there has not been a uniformity of approach, with Scotland proceeding with a ‘hub model’ that has not been replicated across the rest of the UK. Whilst there are some advantages to devolved approaches to enable tailored approaches, there remain instances where differentiated offers can pose challenges. During COVID-19, some users who received a vaccine in two different devolved nation were unable to receive an accurate vaccination certificate because of issues with data-sharing across health services.43‘Covid in Scotland: ‘I’m double-vaccinated but can’t show the proof’’, BBC News, 8 September 2021 [link] Graph 3. Childhood Vaccine Uptake Across the UK, 2020/21 Source: Childhood Vaccination Coverage Statistics, NHS Digital [link] |
Recent Developments in Immunisation Governance
The health and care system in England experienced a large-scale reorganisation in April 2013 following the implementation of 2012 Health and Social Care Act (HSCA).44For an independent assessment of these reforms, see David Buck, The English local government public health reforms: An independent assessment, The King’s Fund (January 2020) [link] A national tripartite delivery framework involving the Department of Health (DH), NHSE and Public Health England (since split to form UKHSA and OHID) was agreed, and a new local operational model was established.
The reorganisation, in particular the delegation of functions had an impact on the distribution of responsibilities for immunisation. Under the pre-reform structure, Primary Care Trusts (PCTs) were accountable to DH and commissioned the majority of services for local geographical areas. This traditional vertically orientated structure meant that a single organisation was responsible for the commissioning, coordination, and evaluation of immunisation. In 2013 PCTs were replaced with general practitioner-led Clinical Commissioning Groups (CCGs). The responsibilities of former PCT functions, such as immunisation coordinators, immunisation programme managers, who played a significant role in supporting and performance managing the programme at the local level were in 2013 distributed among various agencies, often covering larger geographies. Local authorities were also required to work with Primary Health England, which was established in 2013 as a new executive agency of the DH, that incorporated the core health protection functions of the former Health Protection Agency, and local partners to ensure that threats to health, including vaccine preventable strategies, are addressed and that right preventative strategies are in place. This included providing ‘assurance’ for the immunisation programmes that were now commissioned by NHS England.
The national delivery framework
The immunisation programme was then managed through a tripartite (DH, NHSE, and PHE) national delivery framework and a local operating model. The national framework assigned DH responsibility for providing national strategic oversight, NHSE responsibility for commissioning services and PHE responsibility for providing scientific support. Commissioning intentions and budget requirements for the delivery of the immunisation programme are decided annually by DH and NHSE and published in a public health functions agreement referred to as Section 7a.45NHS public health functions (section 7A) agreement 2021 to 2022: letter from DHSC to NHSE, Department of Health & Social Care, 18 November 2021 [link] This legal agreement is approved by the NHSE Board and Secretary of State. PHE supported DH and NHS England in system leadership and planning and held specific responsibilities for the implementation of the immunisation programme, the provision of service specifications for individual vaccine programmes, the procurement of vaccines, and the provision of specialist advice and information at national and local level.
The local operating model
At a local level, PHE employed screening and immunisation teams (SITs) embedded within NHSE Local Teams covering different geographic areas. SITs were accountable to both the PHE and NHSE. SITs were tasked with providing local leadership, encouraging multi-agency working, ensuring high quality delivery of programmes based on national specifications, supporting commissioning, providing advice to the public and health professionals, and monitoring the performance of community and primary care providers. CCGs, on the other hand, were expected to support SITs particularly with quality improvement in primary care.
Local government was responsible for offering independent scrutiny of the local immunisation programme delivery, making sure that it is responsive to local population needs, and commissioning community health services, which can include immunisation activities. Specialist health teams headed by a Director of Public Health were established within local government offices, or local authorities (LAs) and positions are mainly filled by previous PCT public health staff.
Table 3. Overview of recent restructuring of immunisation programmes
| Key system component | Pre-2012 HSCB reforms | Post 2012 HSCB reforms | PHE reform – 2020/21 |
| Policy development, advice to ministers | Department of Health (national) | Department of Health (national) | Department of Health and Social Care (national)
|
| Vaccine Procurement | Department of Health (national) | Public Health England (national) | UKHSA (national)46Elizabeth Rough, Research Briefing: UK vaccination, House of Commons Library, 7 March 2022 [link] |
| Commissioning | Primary Care Trust (local) | NHS England (national) | NHS England (national) |
| 16 national programmes
School based programmes |
Local authorities (local) or NHS England (national)
|
Local authorities (local) or NHS England (national)
|
|
| Disease surveillance/Outbreak response | Health Protection Agency (national) | Public Health England (national) and NHS England (national) | UKHSA (national) |
| Advocacy, communication and health promotion | Primary Care Trust (local) | Public Health England (national) | UKHSA (national)
OHID (national) |
| Local authorities (local) | Local authorities (local) | ||
| System coordination | Primary Care Trust (local) | NHS England (national) | NHS England (national) |
| Vaccine Delivery | General Practitioners (local), NHS Community Trusts (local), other providers (local or national) | General Practitioners (local), NHS Community Trusts (local), other providers (local or national) | General Practitioners (local), NHS Community Trusts (local), School Immunisation Team (local), other providers (local or national) |
| Child Health Information System (CHIS) and Data management | Primary Care Trusts through Child Health Information Systems (local) | Child Health Departments through CHISs (local) | Child Health Departments through CHISs (local)
|
| Workforce training | Primary Care Trusts (local) | Health Education England (national) | Health Education England (national) |
| Others: Needs assessments, scrutiny, and system assurance. | Primary Care Trusts (local) | Local Authorities (local) | Local Authorities (local)
|
| Others: Quality improvement (Duty of) | Primary Care Trusts (local) | Clinical Commissioning Groups (CCGs) (local but give assurance to NHS England) | Former Clinical Commissioning Groups (CCGs)
|
Source: Tracey Chantler & Saumu Lwembe et al., “It’s a complex mesh”- how large-scale health system reorganisation affected the delivery of the immunisation programme in England: a qualitative study’, BMC Health Services Research (2016), 1-14 [link]
Prior to April 2013, the English immunisation programme was amongst the highest performing in advanced economies, with 94.7% of infants received first dose of DTap/IPV/Hib. As Policy Exchange has examined previously, major reforms to a tripartite system architecture governing immunisation have not produced improved outcomes.47Richard Sloggett, ‘Saving a lost decade: How a new deal for public health can help build a healthier nation’, Policy Exchange (November 2020) [link] The changes occurred meanwhile in the context of significant programmatic changes with the addition of rotavirus (2013) and shingles (2013) vaccines to the routine schedule. Dispersed decision-making and uncertainties regarding funding remain significant challenges.48E. W. Gadsby & S. Peckham et al., ‘Commissioning for health improvement following the 2012 health and social care reforms in England: what has changed?’, BMC Public Health, Vol 17, No. 211 (2017) [link] A report by the Royal Society for Public Health recently concluded that the reforms were responsible for lower rates of immunisation.49‘Legacy of 2012 Act to blame for low flu vaccine rates in London’, Royal Society for Public Health, 18 February 2021 [link] Other studies have supported this view.50Tracey Chantler & Saumu Lwembe et al., “It’s a complex mesh”- how large-scale health system reorganisation affected the delivery of the immunisation programme in England: a qualitative study’, BMC Health Services Research (2016), 1-14 [link] A recent National Audit Office however claims that “many of these issues” (resulting in declining performance) “have been known for several years and cannot be reliably linked to the decline in uptake rates since 2012-13”, citing access to GPs and problems with the completeness of the reported data.51Investigation into pre-school vaccinations, National Audit Office, 25 October 2019 [link] (p. 9)
Post 2013
In the Summer of 2018, the Minister for Public Health and Primary Care requested a “fool proof” plan from Public Health England and NHS England to reverse the decline and to reduce regional variation. Various initiatives have been trialled since then to improve uptake, such as changing how NHS England commissions vaccination services from GPs and by providing more regular updates to Ministers. In July 2019, in the Prevention green paper, the Department announced that it would launch a new strategy on vaccination by spring 2020 that included some of these actions.52Ibid.
Table 4. Changes to Public Health Commissioning, 2002-22
| 2002 | Primary Care Trusts (PCTs) assume responsibility for commissioning public health
Management of NHS community health services, such as district nursing, health visiting and children’s services |
| 2003 | The Health Protection Agency is established
Taking over infectious diseases from health authorities |
| 2011 | Healthy lives, Healthy People
Command paper establishes principles for Health and Social Care Act53Healthy Lives, Healthy People: Update and way forward (July 2011) [link] |
| 2012 | The Health and Social Care Act
Introduces major changes to the commissioning and delivery of public health:
|
| 2013 | Primary Care Trusts Abolished
Replaced by Clinical Commissioning Groups (CCGs), and nationally led by a new independent NHS Commissioning Board (now called NHS England) |
| 2021 | Dissolution of Public Health England
Creation of two bodies its place: UKHSA and OHID |
| 2022 | Health and Care Act
Places integrated care systems on a statutory footing, dissolving CCGs |
1.1 How are vaccines currently delivered in England?
Routine immunisation programmes are primarily delivered through the following providers: general practice (GPs), community pharmacy, and School-Age Immunisation Services (SAIS). Local government (through the Director of Public Health, local resilience forums and health protection boards) play a key role in public health protection more widely.
General practice
The majority of vaccines are currently delivered by general practice – most often by practice nurses.55Anthony Harnden, ‘COVID-19 vaccination programme: a central role for primary care’, British Journal of General Practice, vol. 71, No. 703 (2021), 52–53 [link] General practice is well-suited (and often well-placed) to vaccinate effectively given their embeddedness in communities, the fact GPs are trusted healthcare professionals who provide relationship-based care; operate from regulated premises with cold storage systems and resuscitation equipment; and hold patient records for which they are responsible, meaning they are well placed to call and recall individuals for vaccination.56Simon Hodes, Sian Stanley & Azeem Majeed, ‘A national vaccination service for the NHS in England: a proposal to be considered with caution’, BMJ, 7 February 2022 [link]
New delivery models during COVID-19 were developed based on existing local knowledge, and networks fostered by general practice.57Helen Skirrow, Charlotte Flynn & Abigail Heller et al., Delivering routine immunisations in London during the COVID-19 pandemic: lessons for future vaccine delivery. A mixed-methods study’, BJGP Open, Vol. 5, No. 4 (2021) [link] This is one of the principal reasons why COVID-19 jabs were delivered in high numbers in general practice and represented better value for money than other settings (such as mass immunisation centres).58The rollout of the COVID-19 vaccination programme in England, National Audit Office, 25 February 2022 [link]; Helen Salisbury, ‘Why we should keep jabs local’, BMJ vol. 378, no. 1852 (2022) [link]
Since 2019, almost all GP practices have worked as primary care networks (PCNs) (of between 30,000 to 50,000 patients). These organisations represent a beneficial scale for immunisation and there is a clear opportunity to use PCN footprints to develop ‘Integrated Neighbourhood Teams’ – one of the cornerstones of Dr Claire Fuller’s recent ‘stocktake’.59Next steps for integrating primary care: Fuller stocktake report, NHS England (May 2022) [link] Some PCNs worked with neighbouring PCNs to use larger sites such as sports centres and entertainment venues for vaccination and many established “pop-up clinics” example in homeless shelters, community centres, places of worship, and hostels—with great success.60Simon Hodes & Azeem Majeed, ‘Building a sustainable infrastructure for covid-19 vaccinations long term’, BMJ, vol. 373, no. 1578 (2021) [link] Moreover, ‘continuity of care’ provided by general practice is another factor which can boost adherence, and can assist in vaccine uptake, improving trust where hesitancy or uncertainty may be a factor. General practice teams also lead on housebound immunisations.53
In general practice, the following themes have been associated with high influenza vaccination uptake (with applicability across the routine schedule) including leadership (a named lead), ordering sufficient vaccines, keeping up-to-date registers of patients at risk, starting programmes early, enabling robust call and recall, offering appointments and opportunistic vaccination, and working with community midwives for vaccination during pregnancy. A study in BMJ Open stated that if widely implemented across general practice, uptake rates would increase by 7-8%.61Laura J Dexter & M Dawn Teare, ‘Strategies to increase influenza vaccination rates: outcomes of a nationwide cross-sectional survey of UK general practice’, BMJ Open, Vol. 2, No. 3 (2012) [link] Financial targets also appear to incentivise practices to work harder to maximise seasonal influenza vaccine .52
There is however a high level of variation in how GP practices in England implement programmes.62Tim Crocker-Buque, Michael Edelstein & Sandra Mounier-Jack, ‘A process evaluation of how the routine vaccination programme is implemented at GP practices in England’, Implementation Science, Vol. 13, No. 132 (2018) [link] A July 2018 study undertaken by South, Central and West (SCW)’s Improving Immunisation Uptake Team Initiative explored variation in uptake across the Thames Valley Child Health Information Services (CHIS). Their findings were as follows63Improving Immunisation Uptake Team Initiative, South, Central and West (SCW) [link]:
- Many practices did not have a clinical/admin immunisations lead. Even in practices where there was a named lead, their role and responsibilities were not clearly defined;
- Many Practice Nurses (and some Practice Managers) were unaware of their immunisation uptake rates;
- Vaccines being given too early was commonplace in some practices;
- Availability and flexibility of immunisation appointments was a common challenge identified by both staff and parents;
- Many practices did not fully understand the role of Child Health Information Services and their processes/data requests;
- There was a recognition that more effective programmes for GPs to work with other providers, such as school nursing teams (and wider educational leadership) were required
Increased demand for GP services has prompted a debate about whether suspending “non-essential work” in general practice in order to undertake vaccination campaigns is appropriate. In a recent editorial in Pulse, “vaccinations” were cited as “one of the chunks of work” which GPs ought to consider a “necessary sacrifice” to reduce unsustainable workloads.64 ‘When do we admit defeat?’, Pulse, 4 July 2022 [link] In some instances, swift changes to the national approach in recent years has added pressure upon GP services to adapt delivery models and to conduct call and recall at particularly short notice.65Nick Bostock, Last-minute expansion of COVID-19 and flu jabs threatens ‘severe problems’ for GPs’, GP Online [link] Other factors that will influence the ability to maximise the role of general practice include payment for vaccination (practices will now receive a £10.06 item of service fee for Covid-19 vaccinations, whereas in previous phases they received £12.58 per jab, whilst practices will also no longer receive additional payments for care home vaccinations).66Emma Bower, ‘BMA raises ‘serious concerns’ about GP workload and funding for autumn COVID boosters’, GP Online [link]
In Scotland, an alternative ‘hub’ model approach was introduced in 2018 with the explicit purpose of reducing GP workloads. Some queried moving the programme across to health boards wholesale, and development of the scheme has been partially delayed by the pandemic, yet it has already demonstrated some success in boosting uptake, whilst also revealing challenges in introducing a more centralised service.67See for instance, case study in Western Isles indicating 6% increase in uptake: Vaccination Transformation Programme in Remote and Rural Western Isles’, Health Improvement Scotland [link]; On concerns, see Henry Anderson, ‘GPs question transfer of vaccinations to health boards’, Healthandcare.scot, 1 November 2021 [link]; Argyll & Bute HSCP for instance had to apologise for “a considerable number of errors in communication of available clinics and appointment letters” that led to public ”uncertainty, anxiety and inconvenience” in October 2021.68Esmé Pringle, ‘National vaccine system a “challenge” for rural areas’, Healthandcare.scot, 26 November 2021 [link]
Ultimately, a new balance between supporting the holistic care general practice provides coupled with a greater proportion of transactional vaccinations take place across some programmes may be required, but we have concluded that it would be unwise to replicate the Scottish hub model in England at the present time.
| Box 2. How is General Practice Reimbursed for Immunisation |
| In 2004, the new General Medical Services (GMS) contract defined vaccination and immunisation as ‘Additional Services’: one for childhood vaccinations; and the other for adult vaccinations. All routine childhood immunisations, travel vaccines, a small number of adult vaccines were included. Practices could choose to opt out of the delivery of these services, but a reduction in the Global Sum (of 1-3%) resulted. Additional Services supplemented by two Directed Enhanced Services (DES): the Childhood Immunisation Scheme and Seasonal Influenza vaccination more recently.
From April 2021 however, the 2021/22 GP contract saw vaccinations and immunisations become an essential service with item of service fees set at £10.06, and four new indicators covering vaccinations and immunisations added to the Quality and Outcomes Framework (QOF), replacing the childhood immunisation DES.69Costanza Potter, ‘GP vaccine incentives could have ‘unintended consequences’ on other jab uptake, NICE warns’, Pulse, 18 May 2022 [link] In sum:
These stricter targets have seen some GP practices better renumerated for their immunisation activity, but some practices also stand to lose in income from child immunisations. It was recently reported that one practice is set to lose £66,000 a year.71Caitlin Tilley, ‘Some GP practices face losing up to £66k in child immunisation payments’, Pulse, 5 April 2022 [link] Some GP practices have threatened to reduce or to avoid delivering immunisations as a result.72‘QOF: Practices consider viability of offering childhood immunisations’, Management in Practice, 14 April 2022 [link] |
Community pharmacy
Community pharmacy represents – as a recent analysis puts it – “a strategically important setting with great potential to deliver services aimed at promoting health, and preventing disease”.73Katie Thomson Frances Hillier-Brown & Nick Walton et al., The effects of community pharmacy-delivered public health interventions on population health and health inequalities: A review of reviews, Preventive Medicine, Vol. 124 (July 2019), 98-109 [link] In many countries, community pharmacy is the most accessible healthcare provider to the general public: they are available without an appointment; are open evenings and weekends; are located for the majority of the population within a twenty-minute walk; and access is greater in areas of highest deprivation, meaning there is ‘a positive pharmacy care law’.74Adam Todd, Alison Copeland & Andy Husband, ‘The positive pharmacy care law: an area-level analysis of the relationship between community pharmacy distribution, urbanity and social deprivation in England’, BMJ Open (2014) [link]; Youssef M. Roman, ‘COVID-19 pandemic: the role of community-based pharmacy practice in health equity’, International Journal of Clinical Pharmacy, Vol. 44 (2022), 1211–1215 [link] As both retail outlets and care settings, with over 11,500 currently in England, these settings located on high streets or in supermarkets or shopping centres, provide accessible, essential services (such as medication dispensing) and enhanced services (such as vaccination).75Future of community pharmacies – Research Briefing, House of Commons Library, 20 June 2022 [link] In recent years they have increasingly been commissioned to provide seasonal flu and adult pneumococcal (PPV23) vaccines (and more recently, COVID-19 vaccination).76Ian Maidment, Emma Young & Maura MacPhee et al. ‘Rapid realist review of the role of community pharmacy in the public health response to COVID-19’, BMJ Open, Vol. 11, No. 6 (2021) [link] Many pharmacies will also offer private vaccination services, with a focus on travel vaccination.
Policy makers have long seen the benefit of offering routine vaccinations ‘on the high street,’ as an accompaniment to the work of general practice.77Aya F. Ozaki, Christine L. Cadiz & Keri Hurley-Kim et al., ‘Worldwide characteristics and trends of pharmacist interventions contributed to minimize health disparities’, Clinical Pharmacy Forum, Vol. 5, No. 8 (August 2022), 853-864 [link]; Katie Thomson, Frances Hillier-Brown & Nick Walton, ‘The effects of community pharmacy-delivered public health interventions on population health and health inequalities: A review of reviews’, Preventive Medicine, Vol. 124 (July 2019), 98-109 [link] In both the Republic of Ireland and Canada, community pharmacy has become an integral part of campaigns with pharmacists participating in “planning, pharmacy regulators provide clear guidance on vaccination management and vaccinations are equitably refunded through public health systems”.78Fiona Ecarnot, Gaetano Crepaldi & Philippe Juvin et al., ‘Pharmacy-based interventions to increase vaccine uptake: report of a multidisciplinary stakeholders meeting’, BMC Public Health, Vol. 19, No. 1698 (2019) [link] This is not yet commonplace internationally, however. A 2016 study from the International Pharmaceutical Federation shows the great international variability in the roles and responsibilities pharmacists play.79An overview of current pharmacy impact on immunisation: A global report 2016, International Pharmaceutical Federation [link]
Indeed, in England barriers to boosting the role of community pharmacy remain. Pharmacists are not commissioned by NHS England deliver more than a small number of vaccines.80Adam Pattison Rathbone, Wasim Baqir & David Campbell, ‘Barriers and enablers to pharmacists’ involvement in a novel immunisation programme’, Exploratory Research in Clinical and Social Pharmacy, Vol. 7, September 2022 [link] Rather than seamless cooperation, there are challenges with – as the Murray Review put it – “poorly developed local relationships between professionals…[which] inhibit[s]…integration and wider engagement.”81Richard Murray, Community Pharmacy Clinical Services Review 2016 [link] GPs have raised concerns about the potential negative impacts on clinical management, data flows, funding for practices and efficiency of service delivery due to ‘vaccine wastage’ when immunisation occurs in community pharmacy.82Katherine Atkins, Albert Jan van Hoek, Conall Watson, ‘Seasonal influenza vaccination delivery through community pharmacists in England: evaluation of the London pilot’, BMJ Open, Vol. 6, No. 2 (2016) [link] But these challenges are not exclusive to England. A recent study from Switzerland found a lack of uniform regulation for vaccination in pharmacies posed challenges for interprofessional cooperation.83Meliha Jusufoska, Marta Abreu de Azevedo & Josipa Tolic et l. “Vaccination needs to be easy for the people, right?”: a qualitative study of the roles of physicians and pharmacists regarding vaccination in Switzerland ‘, BMJ Open, Vol. 11, No. 12 (2021) [link]
A recent study in the Journal of Public Health which identifies twenty-eight evaluations of pharmacy immunisation programmes in the UK finds “weak evidence of widening access to individuals who had not previously been vaccinated”. Whilst the evidence found that pharmacies were deemed acceptable and convenient venues for vaccination, their cost-effectiveness was not assessed.84S Perman, R M Kwiatkowska & A Gjini, ‘Do community pharmacists add value to routine immunization programmes? A review of the evidence from the UK’, Journal of Public Health, Vol. 40, No. 4 (December 2018), e510–e520 [link] Another study in the British Journal of General Practice which examines the contribution of community pharmacy toward influenza vaccination in Wales found that pharmacy reached younger at-risk individuals, in whom vaccine uptake was lower in greater proportion than influenza vaccination programmes as a whole. Extended opening hours and urban locations were positively associated with the number of vaccinations given, although pharmacists interviewed reported that “workload, vaccine costs, unforeseen delays, lack of public awareness, and GPs’ views of the service limited their contribution.” Pharmacists, aware of the potential for conflict with GPs, moderated their behaviour to mitigate such risk. Another study finds that pharmacy flu vaccination services complement those provided by GPs to help improve overall coverage and vaccination rates in at-risk groups, with services highly accessed by consumers from all socio-demographic areas, and particularly attractive to carers, frontline healthcare workers, and those of working age.85Meliha Jusufoska, Marta Abreu de Azevedo & Josipa Tolic et l. “Vaccination needs to be easy for the people, right?”: a qualitative study of the roles of physicians and pharmacists regarding vaccination in Switzerland ‘, BMJ Open, Vol. 11, No. 12 (2021) [link] Another study found an increase in vaccine coverage when pharmacists were involved in the immunisation process, regardless of role (educator, facilitator, administrator) or vaccine administered (e.g., influenza, pneumococcal), when compared to vaccine provision by traditional providers without pharmacist involvement.86J.E. Isenora, N.T. Edwards & T.A. Alia, ‘Impact of pharmacists as immunizers on vaccination rates: A systematic review and meta-analysis’, Vaccine, Vol. 34, No. 47 (11 November 2016), 5708-5723 [link] Evidence suggests pharmacists can also play a key role as information counsellors, supporting patients with vaccine hesitancy. 87Youssef M. Roman, ‘COVID-19 pandemic: the role of community-based pharmacy practice in health equity’, International Journal of Clinical Pharmacy, Vol. 44 (2022), 1211–1215 (2022) [link] A study of a London-based pilot found that pharmacy-administered flu vaccine doses costed the NHS up to £2.35 less than a dose administered at a GP, with potential for improving convenience for vaccine recipients. However, that same study also found “the use of two separate recording systems leads to time-consuming data entry and missing vaccine record data.”88Katherine Atkins, Albert Jan van Hoek, Conall Watson, ‘Seasonal influenza vaccination delivery through community pharmacists in England: evaluation of the London pilot’, BMJ Open, Vol. 6, No. 2 (2015) [link] As the Murray Review found, the “greater digital maturity and interconnectivity to allow pharmacy staff to see, document and share clinical information about patient care with the clinical records held by other healthcare professionals” is required.89Richard Murray, Community Pharmacy Clinical Services Review (2016), p. 8 [link]
School Age Immunisation Services (SAIS)
School Age Immunisation Services (SAIS) are commissioned by NHS England Regional teams to deliver the school-age routine immunisation schedule and also to visit schools during the Autumn Term to offer flu vaccination.90Health protection in children and young people settings, including education, UK Health Security Agency [link] Providers are contractually responsible for the following programmes: Human Papilloma Virus (HPV), Diphtheria, Tetanus and Polio (Td/IPV), Meningococcal ACWY (MenACWY), Measles, Mumps and Rubella (MMR) and Flu Nasal Vaccinations.
Most effectively deployed, clinical work is supported by the delivery of lessons to promote the importance of immunisation, with schools nominating a staff member to act as a link person for the SAIS. It is not clear how widespread this best practice currently is, however. Typically, the nominated teacher will help coordinate preparatory lessons and the planning and delivery of the services, including the consent process, which typically requires verbal or written confirmation from a parent or guardian for a child or adolescent aged under the age of 16. By law, some young people can be mature enough to provide their own consent, and therefore the Gillick competence can determine whether a child can be considered competent enough to understand the benefits and risks of vaccination.91‘Gillick competency and Fraser guidelines’, NSPCC Learning, 5 August 2022 [link]
Evidence from a wide range of studies shows that school-based vaccination is effective in achieving high uptake and completion rates (and, when commissioned, can effectively support the delivery of catch-up doses such as for MMR).92Proma Paul & Anthony Fabio, ‘Literature review of HPV vaccine delivery strategies: considerations for school- and non-school based immunization program’, Vaccine, Vol. 32, No. 3 (2014) [link]. On the value of commissioning for catch-up programmes, see F Altinoluk-Davis, S Gray & I Bray, ‘Measuring the effectiveness of catch-up MMR delivered by school nurses compared to signposting to general practice on improving MMR coverage’, Journal of Public Health, Vol. 42, No. 2 (June 2020), 416–422 [link]
Research also reveals that school-based vaccination is successful in reducing the burden of disease in the wider community.93Sarah Perman, Simon Turner & Angus I. G. Ramsay et al., ‘School-based vaccination programmes: a systematic review of the evidence on organisation and delivery in high income countries’, BMC Public Health, Vol. 17, No. 252 (2017) [link]
Local Government
Local Government has – following the Health and Care Act 2012 – had an expanded responsibility to lead on major health issues. Each unitary Local Authority (LA) must employ a specialist Director of Public Health (DsPH). These individuals are accountable for the delivery of their authority’s public health duties, with a remit for health improvement and health protection. As of September 2021, there were 135 DsPHs across 153 LAs (in several instances, such as in Northamptonshire, two LAs have entered into shared arrangements to optimise the public health offering).94Guidance – Directors of public health in England, Public Health England, 7 September 2021 [link] For screening and immunisation programmes, DsPHs are expected to provide appropriate scrutiny and challenge to arrangements, alongside advocating for interventions which reduce health inequalities.95Directors of Public Health in Local Government: Roles, Responsibilities and Context, DHSC, January 2020 [link]
On the one hand, DsPHs have a formal role in the local public health system; they have helped guide and shape the response within regional and local emergency structures and committees. On the other hand, they engage a wide range of stakeholders, including across local communities, facilitating vital social support.96Shilpa Ross, Deborah Fenney, Clair Thorstensen-Woll & David Buck, Directors of public health and the Covid-19 pandemic – ‘A year like no other’, The King’s Fund (September 2021) [link] The recent pandemic demonstrated the value of this convening power.97Ibid.
In his recent review of approaches taken to support the rollout of COVID-19 vaccines, Nicholas Timmins says that “local authorities did many things, from the seemingly small – for example, suspending yellow lines and parking bays outside vaccination centres – to finding vaccination sites, supporting mobile vans (see Box 8 of an example of such working, predating the pandemic), and leading big drives to build trust in the vaccine and spread the word.”98Nicholas Timmins & Beccy Baird, The Covid-19 vaccination programme: Trials, tribulations and successe, The King’s Fund, January 2022 [link], p. 54
Positive engagement with local government enabled the best use of local assets to boost uptake – particularly the use of traditionally non-medical spaces, such as leisure centres or faith centres. There is a risk however – both due to a declining urgency post-pandemic, coupled with shortages in local public health expertise which could undermine the positive steps taken during the pandemic.
| Box 3. A ‘Mobile Clinic’ – Slough Borough Council |
How and why it worked
|
| Box 4. International Best Practice: Delivery Models | ||||||||||
|
Next chapter
Chapter 2: How have recent outbreaks impacted immunisation policy?
2.1 The Impact of COVID-19
The pandemic has significantly impacted national routine immunisation programmes. Globally, the WHO and UNICEF have recorded the largest decline in childhood immunisation in 30 years. The percentage of children receiving three doses of the diphtheria, tetanus and pertussis (DTP3) fell 5% points between 2019 and 2021, equivalent to 23 million children missing out100COVID-19 pandemic fuels largest continued backslide in vaccinations in three decades, WHO, 15 July 2022 [link] . Early in the pandemic, advice from the JCVI stated children should continue to receive vaccinations however, restrictions placed on movement and non-essential travel did result in a decline in uptake. School closures also forced the operational delivery of all school-aged immunisation programmes to pause temporarily. For instance, the adolescent Td/IPV vaccine coverage amongst the Year 9 cohort dropped significantly to 57.6% in 2019/2020, from the pre-pandemic levels of 87.6% in 2018/2019.101Tetanus, diphtheria and polio (Td/IPV, ‘school leaver booster’) vaccine coverage for the NHS adolescent vaccination programme in England, academic year 2020 to 2021– Health Protection Report, UKHSA, Vol. 16 No. 2 (8 February 2022) [link]
Graph 4 shows the change in childhood immunisation coverage pre-pandemic (Jan-Mar 2020) and during (Jan-Mar 2022) across the four devolved nations. In general, Wales had the highest declines across the five selected routine programmes. PCV booster coverage saw the sharpest decline in all countries, with Wales and England witnessing a fall of 1.7% and 1.6% respectively. Scotland however saw an increase in immunisation coverage in all programmes apart from the PCV booster. A study in Scotland also found similar trends––with differences ranging from 1.3% for first dose 6-in-1 vaccine to 14.3% for second dose of MMR. 29 The study stated that although it was not possible to identify the causes, flexible working during lockdown may have made it easier for parents to attend vaccination appointments. Other reasons could include easier access to vaccination centres and mobile centres as well as direct communications with families to remind their upcoming vaccinations schedules.
Graph 4. Change in childhood immunisation coverage between Jan-March 2020 to Jan-Mar 2022
Source: Cover of vaccination evaluated rapidly (COVER) programme, quarterly data, NHS Digital [link]
Coverage similarly dropped for adult immunisations, such as Shingles (recommended for those aged between 70 and 79).102Shingles vaccine coverage report (adults eligible from April 2020 to March 2021 and vaccinated to the end of September 2020, December 2020, March 2021, and June 2021): England Annual report of the financial year 2020 to 2021, Health Protection Report, UKHSA, Vol. 16 No. 4 (29 March 2022) [link]
The public health impact of slow catch up on immunisation coverage is substantial. To quantify this impact further, we undertook two case studies to better understand and demonstrate the public health impact to reduced uptake and delay in terms of incidences and mortalities. We found that by increasing the coverage of two doses of MMR (measles) from the current 87% to WHO’s target of 95%, an estimated 936 cases a year could be prevented (See Box 4). We also estimate that an increase from the current 65% to 85% uptake of shingles vaccine could prevent 4168 cases of shingles, 1370 cases of PHN, and 75 hospitalisations annually (See Box 5).
| Box 5 – Impact of a slow catch up: Measles | ||||||||
| After several decades of rising coverage, the past decade has witnessed multi-year reductions in core childhood vaccines such as measles, mumps, and rubella (MMR) and diphtheria, tetanus, pertussis and polio (DTaP/IPV) vaccines. These reductions in coverage are of particular concern because of the considerable rise in measles affecting other European countries.103Tim Crocker-Buque, Kitty Mohan & Mary Ramsay et al., ‘What is the cost of delivering routine vaccinations at GP practices in England? A comparative time-driven activity-based costing analysis’, Human Vaccines & Immunotherapeutics, Vol. 15, No. 12 (2019), 3016–3023 [link] Between 2016 and 2018, an average of 72 measles cases in the UK are imported, mostly from Europe, and initiated outbreaks of different scales104Measles and rubella elimination country profile: United Kingdom of Great Britain and Northern Ireland, WHO [link].
To estimate measles incidence, we used a linear regression model to predict measles cases based on the region’s MMR coverage rate using data from 2013 to 2019. The regression analysis estimates that if measles coverage remains at a current level (as of date 30 Sep 2021) of 87%, the estimated incidence of measles would be 1,026 (± 2.98) per year, whereas the figure reduces to 90 (± 2.98) when the coverage rate is set to 95%. That is, by increasing MMR second dose uptake to 95%, there is a potential to prevent 936 measles cases per year. Table 5. Summary of estimated outcome
|
| Box 6 – Impact of a slow catch up: Shingles | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Live attenuated herpes zoster (HZ) vaccination was first used on 1 September 2013, in 70-79-year-olds. The average vaccination rate for shingles in 2020/2021 was 65%. Furthermore, Shingles coverage rates were 40.6% as of March 2022. The pandemic has further exacerbated the low uptake of shingles vaccine. While shingles is rarely life-threatening, resulting pain can be constant and severe, drastically decreasing the quality of life and sometimes, resulting in hospitalisation.
This exercise estimates the difference in annual cases of HZ between a coverage rate of 65% (current average as of 23 March 2022) and 85% in England in year 2020/21 (latest statistics). The population included in the study is that aged between 70 and 79 years old, as the vaccine is currently only administered to those in this age group. We also estimate the annual cases of hospitalisation, deaths, and Quality-Adjusted Life-Years Loss due to HZ and Post Herpetic Neuralgia (PHN). Results Table 6. 3 Estimated public health outcomes with 65%, 75%, and 85% shingles vaccine coverage (population aged 70-79)
Table 7. Summary of Estimated Outcomes (population aged 70-79)
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||
2.2 A Cost Analysis of Vaccine Delivery Across Different Sites During COVID-19
The choice of vaccination sites has implications for accessibility, trust, safety and equity. Pop-up services may be highly effective in increasing accessibility and convenience (whilst removing the need to book), but creates a system that is more transactional, whilst there are additional complexities to administering vaccines beyond traditional clinical settings.
In Graph 5, the National Audit Office’s recent report on the economic evaluation of COVID-19 rollout broke down the demographic composition of those vaccinated across three different channels: hospitals – despite bearing the highest vaccination costs per dose delivered105The rollout of the COVID-19 vaccination programme in England, National Audit Office, 25 February 2022 [link] – played an important role for the population over 80 years old and frontline workers; local vaccination services on the other hand were the most popular and cost-effective vaccination sites across all age groups––between 60% and 97% of population received their vaccine through either general practice, community pharmacy, or other mobile options. Mass vaccination centres were anticipated to be the main hub for COVID-vaccination, delivering between 1% to 37% of doses across all groups and being the most widely used route for those aged 65 years and below.
NHS England initially planned on the basis that 41% of vaccinations would be delivered at vaccination centres; 56% by GPs and community pharmacies and 3% in hospitals. By the end of October, only 21% of first and second doses had been delivered at vaccination centres and 71% by GPs and pharmacies (mostly in general practice, where 56% of doses were administered).
Graph 5. Percentage of vaccine doses delivered for each priority group by delivering model in England, December 2020 to October 2021
Source: The rollout of the COVID-19 vaccination programme in England, National Audit Office, 25 February 2022 [link]
Table 8 Illustrates these cost differentials. Vaccination centres have a higher unit cost, given it is necessary to establish new clinical facilities, such as short-term leases of venues where NHS-owned venues are not available. Recruitment and training of temporary extra workforce to support the administration of vaccines also increased variable costs. Some programme costs cannot be easily quantified as some aspects of the programmes relied on goodwill and support from a variety of individuals and organisations that served as volunteers, or provided venues for free or at reduced rates, meaning some costs would likely be higher were the vaccination programme to continue as part of the routine programme.106The rollout of the COVID-19 vaccination programme in England, National Audit Office, 25 February 2022 [link] Pop-up services are also more costly, as there is a need to establish new clinical facilities, such as renting buses or pop-up venues. The recruitment and training of temporary extra workforce also added extra costs, although during COVID-19 much of the work was carried out with the support of voluntary sectors, such as by St John Ambulance.
Table 8. A Comparison of Different COVID-19 Vaccination Sites
| Target population | Percentage delivered (until October 2021) | Workforce | Ability to provide holistic approach | Cost Implications for COVID-19 vaccines | |
| Vaccination Centre | Mobile population (18-64)107The rollout of the COVID-19 vaccination programme in England, National Audit Office, 25 February 2022 [link] | 21% | GPs, practice nurses, pharmacists,
Volunteers |
Weak
|
£34 (NAO, 2022, 50) |
| Hospital Hubs | Frontline workers, population needing secondary, tertiary scare, population > 80 108Ibid. | 8% | Physicians, practice nurses | Medium |
£18 109Ibid. |
| Local vaccination centres (incl. GP surgeries) | See below | 71% (GPs accounted for 56%) | GPs, practice nurses, pharmacists,
volunteers |
See below | £24 110Ibid.
|
| Local vaccination centres | |||||
| General Practice | Infants and children; general population | 56% (44.5 million) | GPs, practice nurses | Strong | £24111Ibid. |
| Community Pharmacy | General population | 15% | Pharmacists | Medium | £24112Ibid.
|
| Pop Up/
Mobile Services |
Underserved, immobile population | GPs, practice nurses, pharmacists,
Volunteers |
Weak | Additional £5.29 per vaccine (data from case study in Durham) | |
| School Age Immunisation Team | School-aged students | School nurses, Immunisations Nurses | Medium | Commissioned by LAs | |
A cost and outcomes comparison shows that each of the delivery sites are best placed to deliver different vaccination for different population groups. GPs are the most suitable setting for delivering pre-school immunisations with their ability to provide comprehensive, holistic care. Areas with historically underserved populations may find value in mobilising pop-up services to achieve greater coverage.
Immunisation policies need to allow for the differentiation of services based on local characteristics and needs and greater flexibility in immunisation sites options in order to achieve improved outcomes (high coverage and equity) with the lowest costs.
Pop-up or mobile vaccination sites
Typically, mobile, temporary (or ‘pop-up’) vaccination clinics aim to improve access and maximise vaccine uptake in communities with low coverage rates (or those where low coverage is anticipated). A case study from Durham County Council (p. 84) revealed that the cost of delivering the COVID-19 vaccine is estimated to be £5 more than those delivered in general practice. In general, NHSE will provide funding to support reasonable additional costs incurred if contractors organise vaccination sessions off the pharmacy premises, given that there is no other venue that has already been paid for either near or at the same place or other NHS vacant space.113Flu vaccination – Funding and claiming payment, Pharmaceutical Services Negotiating Committee [link] Although the average cost of pop-up and mobile services are higher, additional cost is justified by vaccinating those that are not otherwise able to access vaccination, who tend to be the most vulnerable, immobile, or have frequent contact with the healthcare system.
Careful consideration will therefore be required if such an approach is adopted more widely to ensure cost effectiveness. A four-day festival organised in 2021 to encourage young people in East London to get vaccinated against Covid saw just 435 people jabbed. The event in Langdon Park cost Tower Hamlets Council £237,000 to put on, meaning each vaccine delivered cost £535 – evidently a poor return.114‘Covid vaccine festival cost £535 per person jabbed’, BBC News, 6 April 2022 [link]
2.3 Monkeypox
The recent outbreak of monkeypox (where 98% of the cases are amongst gay, bisexual and queer men) has provided a different health protection challenge compared to the mass population model required for COVID-19.
UKHSA has prioritised ‘men who have sex with men’ for vaccination – at greatest risk are those with multiple sexual partners, group sex participants or attendees at venues such as saunas.115Smrithi Rallapalli, Mohammad S Razai, Azeem Majeed & Simon B Drysdale’, ‘Diagnosis and management of monkeypox in primary care’, Journal of the Royal Society of Medicine, 7 November 2022 [link] Cases have been highest in London, and therefore, sexual health clinics have been deemed the lead organisations for vaccination delivery. Pilots were also introduced during July and August 2022 at sexual health clinics in trusts, including Chelsea and Westminster and Central and North West London to maximise reach. These sites are optimal – given the wider set of supportive services they can also provide – but have also meant there has been difficulty in signposting users to right information (and services) as a result. Some have queried the light touch approach from national authorities, with “each sexual health clinic organising and prioritising patients their own way”, with disparities in access as a result”. One Member of Parliament called for the introduction of a ‘monkeypox tsar’ to coordinate efforts.116Angela Eagle, ‘We must treat monkeypox as a public health emergency to avoid it becoming endemic in the UK’, The House, 8 August 2022 [link] Supply has also proven a challenge. As a result, the JCVI has recently recommended ‘fractional dosing’ to enable more people to receive some protection.117Megan Ford, ‘Smaller doses of monkeypox vaccine to be piloted amid limited supply’, Nursing Times, 22 August 2022 [link] Cases have declined in recent weeks, but the experience overall shows the challenge of coordinating vaccination campaigns across Government at a time where ministers have competing demands.
Next chapterChapter 3: A reformed approach to vaccination and immunisation programmes
This chapter looks at all functions of a successful immunisation programme and proposes a series of suggestions which should be taken forward. Some proposals will be easier to implement (and indeed, there are many examples; others require more fundamental structural change and resource. We will delve into six key elements of immunisation policy, which constitute the following five sub-sections of this chapter:
- Governance and Delivery Models: We explore the potential to establish a National Immunisation Service (NIS) with a centralised booking offer for citizens, whilst considering the benefits associated with separating the policy and operational planning of screening and immunisation services within NHS England. We clarify the differing needs of vaccine programmes: with a need to ensure that childhood vaccinations continue to be delivered – largely – in general practice through the expert supervision of nurses. For adult vaccination, we propose piloting a new delivery model to allow local areas to co-create an optimal model to maximise equity, accessibility, and efficiency. We propose piloting three place-based ‘Vaccination Collaboratives’, which would bring together relevant immunisation providers to collectively deliver immunisation programmes.
- Data: We explore the role for an immunisation information system which supports all immunisation providers, and to enable a ‘single version of the truth’ for the healthcare workforce to monitor progress and mobilise targeted interventions in a timely and accurate manner.
- Workforce: Experience and capacity in the healthcare workforce is a rate-limiting factor in the success of immunisation campaigns and continues to be one of the greatest limiting factors facing the NHS in the short and medium term.
- Engaging Citizens: Users of the immunisation services should be placed at the centre of programme design and delivery to maximise accessibility of services and information, which in turn contribute to increase vaccine uptake. We advocate improved access to health and immunisation records through NHS App to empower users to become active participants in their own health.
- Assessment and Regulations: Several recommendations are made to strengthen the workings of JCVI. These include a greater horizon scanning function and more active public and business involvements that could improve the transparency and processes of the widely-respected JCVI.
3.1. Governance and Delivery Models
“Immunisation struggles from fragmentation…and a significant disconnect between the centre and actual local delivery”
Semi-structured Interview participant 2022
Clarification of leadership and responsibilities across vaccines policy
Recommendation. The Government should set out plans to clarify the national governance and leadership structures for immunisation policy.
The objective is to recognise the complexity of health protection functions, but to clarify responsibilities and to refresh lines of accountability for the delivery with the vaccines minister accountable for overall performance. The existing tripartite arrangements with UKHSA would remain, with the future strategy and approach to industry partnerships aligned to both the Life Sciences Vision and UKHSA’s Scientific Strategy. We also recommend the creation of a National Immunisation Board, chaired by the Vaccines Minister, which would meet (at least) once every six months to scrutinise performance against the WHO target of 95% coverage. Over time we would expect to see consolidation of the role of the NHS England Regions, a redeployment of resource to ICSs and more shared policy work across NHS England and DHSC. This should be gradual rather than immediate given the importance of the catch-up programme and the detrimental short-term impacts that a restructure may create. The Government should also commit to publishing a National Vaccination Strategy in 2023 and every five years henceforth, taking a ‘life course’ approach. It should seek to ensure the recommendations of the latest NICE guideline on improving vaccine uptake are delivered, universally.
Who is ultimately responsible for the successes and failures of immunisation programmes? The current fragmented structure of immunisation programmes does not allow a simple answer to this question. However, this failure to identify a single responsible body for immunisation programme poses a real challenge, as no single authority can ultimately be held accountable for overall performance.
It has been acknowledged for some time that the governance landscape for vaccinations is complex. The reforms following 2012 has created an interplay of organisations. Subsequent reforms, including the creation of new bodies, have added to this process. Some of the key actors responsible for national immunisation programmes (See Figure 2 below) include:
- Department of Health and Social Care (DHSC) – National strategic oversight of vaccination policy in England.
- The Joint Committee on Vaccination and Immunisation (JCVI) – An independent expert advisory committee which advises DHSC (and whose advice the Secretary of State must adopt).
- UK Health Security Agency (UKHSA) – Provides public health oversight of the vaccine programmes and surveillance of vaccine preventable diseases. Other responsibilities include collecting and publishing data on the number of vaccines undertaken, providing clinical advice on delivery, and running procurement and distribution for national programmes.
- NHS England – Has responsibility for delivering the national immunisation programmes under the NHS Public Health Functions Agreement (also known as Section 7A). Commissions services through the GP and pharmacy contracts.
- NHS England Regional Teams – Are responsible for commissioning Providers of School Age Immunisation Services (SAIS) to administer the programme in schools.
- Local Government – Councils are not directly responsible for commissioning or delivering vaccine programmes. Through the local Directors of Public Health they have a role in providing scrutiny and assistance with developing local engagement plans.
- The Office for Health Improvement and Disparities (OHID) is a government unit housed within DHSC, jointly accountable to the Secretary of State for Health and Social Care and the Chief Medical Officer (CMO) for England. OHID was created in October 2021 and leads on public information campaigns on vaccines.
- The Vaccines Taskforce (VTF) was created in May 2020 to meet the desired objective of securing and then distributing a COVID-19 in the shortest possible timeframe. From October 2022, it will become a jointly sponsored unit between the OLS and UKHSA.
Figure 1 (repeated). The Current Governance Architecture of Immunisation in England
Interviews with national level decision-makers and local implementers of immunisation programmes revealed that the tripartite organisational reform where accountabilities are shared between three distinct organisations ‘fragmented the delivery of the immunisation programme’. 137 For example, the reform delegated the management of public health programmes to local government, and embedded PHE-led screening and immunisation teams within local NHS England commissioning bodies. These teams in turn had to create effective working relationships with partners in LA Public Health Teams, CCGs, and PHE Health Protection Teams. One interviewee from LA Public Health Team raised the question, “who’s got that overarching leadership and accountability?” to which he has no answer. This complexity of organisational structures results in stakeholders having to put extra time and effort in coordinating the delivery of immunisation programmes.
Despite the emphasis of joint responsibility, issues emerged about how to manage mutual accountabilities. Our interviews revealed different perspectives about which organisations wielded greatest influence, with some attributing greater command to DHSC, as the delegating authority, and others to NHS England, for its budget assigning responsibility. There is also a confusion about the new role of ICSs, the role of the director of public health in coordinating local responses. In August 2020, the then Secretary of State for Health and Social Care announced that PHE would be abolished and that its public health functions would be transferred to the UK Health Security Agency (UKHSA), whilst its health improvement functions were transferred to the Office for Health Improvement and Disparities (OHID), NHS England, and NHS Digital. Whilst there has been logic and value in creating an explicit singular organisational focus on health protection, this has also had the unintended consequence of muddying the waters on which of OHID and UKSHA is responsible for tackling health inequity.
During interviews we challenged participants to set out suggestions for an alternative structure. Some proposed a return to a typical vertical hierarchy. But many were reticent to recommend wholesale structural changes, recognising that choosing to disband, merge, or create new organisations carries a significant bureaucratic burden and creates uncertainty for the employed workforce.
Our view is therefore to focus upon the following areas:
- Clarifying Remits: During the course of its existence, Public Health England was able to bring together expertise as an executive agency.118David Buck, ‘Public health reform: a whole-government priority?’, The King’s Fund, 1 April 2021 [link] The creation of UKHSA and OHID separates communicable diseases from non-communicable diseases in policy and planning. This has been described in one review as “a serious error because, as the COVID-19 pandemic has shown in stark terms, close links exist between them with regard to the groups and communities who had the highest rates of illness and death during the pandemic”, necessitating close cooperation.119David J Hunter, Peter Littlejohns & Albert Weale, ‘Reforming the public health system in England’, The Lancet Public Health, Vol. 7, No 9 (September 2022), e797-e800 [link] The relationship of UKHSA with the devolved nations, each of which has its own public health agency, must also be clarified.120Ibid. UKHSA already possesses a number of world-leading capabilities – such as in genomic sequencing, but is under-powered in its commercial expertise, necessary to enable it to make the most of its remit. Given UKHSA manages several key national assets for the life sciences sector, such as the recently opened Robinson Building at Porton Down, it is vital these functions are developed.121‘New UKHSA laboratory will ‘define future pandemic response’ with pioneering COVID-19 vaccines and variants research’, gov.uk, 21 February 2022 [link] There is also a need to improve surveillance capabilities. As one of our interviewees put it to us, the surveillance capabilities of UKHSA should be improved so it can “go beyond reactive snapshots…to provide a big-picture predictive view through a health protection lens.”
- Strengthening Lines of Communication: Health protection requires strong partnership working within England with regional public health teams, ICSs, and local government. The processes of UKHSA should reflect these partnerships, and should ensure the integration of Local Government expertise within its functions. There is a need to improve the current interface with local teams. The creation of a Memorandum of Understanding and Framework Agreement, as the Local Government Association has recently advocated is one pragmatic mechanism that may foster closer cooperation.122‘A ‘local first’ public health system’, Local Government Association, 24 February 2021 [link]
Recommendation. Establish a National Immunisation Service (NIS) to modernise vaccination services and to provide wrap-around support to providers.
A National Immunisation Service
When the former Secretary of State for Health and Social Care, the Rt Hon Sajid Javid MP suggested the development of a ‘National Immunisation Service,’ he kickstarted an important debate about the opportunities to capture the learnings from Covid-19 in future vaccination deployments.123Caitlin Tilley, ‘Health secretary proposes ‘national vaccination service’ to relieve GPs’, Pulse, 26 January 2022 [link] NHS England has since stated that “opportunities for alignment and co-administration including catch up across all our vaccination programmes continues” and the “development of a long-term NHS vaccination service has commenced.” Some features have already been developed in recent years, such as the National Immunisation Management Service (NIMS) (profiled in later in this paper), but further plans for a future operating model are forthcoming. 124Costanza Potter, ‘NHS national vaccination service under development’, Management in Practice, 24 May 2022 [link]
An assessment of some of the trade-offs of such an approach are as follows:
Table 9: The possible advantages and drawbacks associated with a National Immunisation Service
| Advantages | Drawbacks |
| Access – Could enable effective scaling of ‘national booking’ across all suitable programmes. Possibility to integrate this function with the NHS App to create option to book, change, or cancel vaccination appointments at a variety of settings. Additionally commissioned services offer the possibility of providing wrap-around services to support existing work of primary care | Premises – Additional cost and regulatory hurdles to clear if new or additional sites commissioned.
|
| Surveillance – England-wide data and coverage information, with a single database automatically triggering paper, text or email invitations and reminder notifications linked to an individual’s NHS number. Much work required however to ensure the accuracy of this information. | Workforce – A newly established national vaccine service may recruit staff from primary care teams, both clinical and non-clinical, thereby further stretching staff in primary care to manage and deliver the programme. |
| Information – Consolidated and consistent information and guides on vaccination safety and efficacy, available in different languages and formats – including BSL, Easy Read, and translations in foreign languages.
Possibilities to improve national communications function to tackle vaccine disinformation and to provide informational support and assets to local teams |
Cost – A piece recently penned in the BMJ challenges “the government to show how this investment in a new service would compare in terms of cost effectiveness with a similar investment in primary care teams.”125Simon Hodes, Sian Stanley & Azeem Majeed, ‘A national vaccination service for the NHS in England: a proposal to be considered with caution’, BMJ, 7 February 2022 [link] |
| Procurement – Ability to improve the distribution network and to create a ‘pull system’ for vaccine supply. Ability to simplify mutual aid and to support access to excess NHS stock (incl. support for late changes to specifications. | Data – Significant fragmentation at present, whilst many centrally held lists contain inaccuracies. Centrally generated COVID shielding lists created additional work for GPs and their teams as they had to clean for accuracy.
A national service would also likely require full access to patients’ electronic medical records which may be challenging given the current controllership rules.126Simon Hodes, Sian Stanley & Azeem Majeed, ‘A national vaccination service for the NHS in England: a proposal to be considered with caution’, BMJ, 7 February 2022 [link] |
| R&D – Building on the work of NIMS and the COVID-19 Registry to support partnerships between life sciences sector and NHS, whilst engaging service users to clinical research. |
Having assessed the advantages and drawbacks we have concluded that bringing all vaccination delivery under a single national system of control would be unwise. The aim of a National Immunisation Service (NIS) should therefore be clarified at the earliest opportunity to reassure providers that it would not represent a ‘total’ delivery model, but instead a ‘wrap-around’ service to complement work being led ‘on the ground’ by general practice (through PCNs), community pharmacy, local government and ICSs in developing ‘evergreen’ immunisation offers.
Its focus – we believe – should be on developing assets and capabilities to support NHS partnerships with the life sciences sector; creating a ‘pull system’ for vaccines by strengthening the role of NHS Shared Business Services (NHS SBS) in working with providers beyond the secondary care sector; clarifying Section 7A arrangements and those vaccines which fall outside it; improving mutual aid between providers and boosting the accessibility of the vaccines programme to users through a diversification of delivery models (led by local teams); and an improved digital offer for booking and accessing information and records. Where the evidence suggests that national delivery models will deliver greater return on investment and improves uptake overall, the NIS should engage in “supplementary immunisation activities” to enable ICS to deliver upon ‘evergreen’ immunisation offers.127C. Edson Utazi, Julia Thorley & Victor A. Alegana et al., ‘Mapping vaccination coverage to explore the effects of delivery mechanisms and inform vaccination strategies’, Nature Communications, Vol. 10, No. 1633 (2019) [link]
Separating Immunisation from Screening
Recommendation. Separate the commissioning responsibilities of screening and immunisation programmes within Section 7A to allow each programmes to be self-managed.
“It was mad that they were put together. Screening is a diagnostic component of a clinical pathway. Immunisation is about health protection”
Semi-structured Interview participant 2022.
How do screening and immunisation services currently interact?
Screening was combined with immunisation under a new single system leadership in 2013. Through the arrangements delegated to NHS England under Section 7a of the HSCA 2012, the NHS England Regions were responsible for commissioning both sets of services on behalf of the Secretary of State. Staff from Public Health England with specialism in either screening or immunisation were then embedded in NHS England Regional teams and nationally to provide accountability and leadership.128Immunisation & Screening National Delivery Framework & Local Operating Model, NHS England, 24 February 2013 [link]
Within different regions, Screening and Immunisations Teams (SIT) were established. Often employed by PHE and housed within the Health Protection Directorate but embedded in NHS England, they support the commissioning of all S7a responsibilities. An example of a typical structure is shown in Fig 3.
Figure 3. Example structure for a regional public health team (adapted from NHS Midlands)
Oversight of S7a is provided through a Public Health Oversight Group, led by NHSE which provides an assessment of the commission and delivery across screening and immunisation programmes. This is supplemented by a S7a Assurance Meeting, which brings together senior officials from DHSC, UKHSA and NHSE. This is the formal accountability meeting for NHSE in its delivery of its statutory public health commissioning responsibilities.
The volumes of activity delivered through this programme are significant. Each year around 20 million children, adolescents and adults will be offered at least one routine immunisation. This is on top of existing COVID-19 vaccine volumes. Meanwhile approximately 11 million new-borns and adults are invited to participate in a screening programme.
Whilst there are similarities which underpin programme delivery, screening and immunisation are distinct clinical disciplines. Screening is a process of identifying apparently healthy people who may be at increased risk of a disease. By contrast, immunisation is process by which a healthy person becomes protected against a disease, often through vaccination. Whilst the former is a designated element of a diagnostic pathway, the latter is about health protection in its widest sense.
Despite their clinical differences, it is possible to see that several of the problems facing immunisation, outlined earlier in this paper, are mimicked in screening. The independent review of screening in England led by Professor Sir Mike Richards concluded that the implementation of S7a had “blurred the lines of ownership and accountability”.129Review of national cancer screening programmes in England, NHS England, 6 February 2019 [link] Professor Richards recommended that the delivery of screening programmes in England should fall solely under NHS England, having observed that the previous model of shared oversight between NHS England and the then Public Health England made data exchange difficult and prone to error. Patient groups with an interest in screening share similar views. In their Computer Says No report, Jo’s Cervical Cancer Trust identified issues with IT systems, alongside fragmented commissioning structures as key explanations why one in four women do not attend cervical cancer screening appointments.130Computer says “no”: The growing issue of access to cervical screening across the UK, the problems and how they can be overcome, Jo’s Cervical Cancer Trust, June 2018 [link]
The case for separation
We have heard from several interviewees that having a combined structure for both screening and immunisations was justifiable in the 2010s but may be deemed inappropriate as we look to the future. Others have been more strident and suggested that they were always poor bedfellows.
The case for change is as much about future proofing as to address current problems. We know that screening is set to change in many ways over the coming decade. The advent of more precise technologies will mean that those at higher risk of a condition can be targeted. Thanks to the genomic revolution, polygenic risk scores will become more accurate and could help inform clinical intervention. We may also see mass population screening programmes, from whole genome sequencing at birth to the ongoing GAIL pilot is exploring the potential to use routine blood testing to detect early cancer in people without any symptoms.131‘NHS to pilot potentially revolutionary blood test that detects more than 50 cancers’, NHS England, 27 November 2020 [link]
Urgent changes will be required to the screening programme. This will need investment, at least up front, and consume significant portions of the scarce change management capacity across the NHS. As we will explore later in this chapter, vaccines are also evolving with a suite of exciting new candidates. Taken together this would represent an optimal moment to separate the two in policy planning, each with their own dedicated leadership structure. We believe it is a separation that would carry mutual benefits for both parties, and signal that both are too important to be competing against each other.
Delivering this change will require close dialogue between NHS England, DHSC and UKHSA, to ensure that the necessary capacity has been identified. Policymakers must also be live to unintended consequences – for example ensuring a strong interface is maintained between HPV vaccination data and cervical cancer screening, given the interrelationship between these two programmes.
In reviewing S7a, the Government and NHS England should review gaps in provision. At the moment there are several vaccines which are either indicated according to the Green Book or within clinical guidance which do not fall under S7a programme delivery. According to a paper by Junghans et al. (2018), these are found in broadly four areas:132Cornelia Junghans, Kerry Lonergan, Catherine Heffernan & Kenny Gibson, ‘Vaccinations not covered under Section 7a: who pays?’, British Journal of General Practice, Vol. 68, No. 667 (2018), 92-93 [link]
- Incomplete vaccination schedules requiring completion, for example MMR in a teenager;
- Vaccination of particular at-risk groups as recommended by the Green Book, for example pneumococcal vaccination for HIV patients, hepatitis B vaccine for a partner of a person infected with hepatitis B or patients with certain long-term conditions;
- Outbreaks of vaccine-preventable diseases where UKHSA recommends mass vaccination as a response, for example MMR within prison;
- As part of individual treatment, for example tetanus vaccine in someone with incomplete immunity following a road traffic accident.
There are a range of further examples too, including patients who have had bone marrow transplants and require a full course of new vaccinations. Ultimately, these current gaps in provision come down to ‘who pays for what’. The costs for these vaccines cannot be claimed under S7a, and therefore former CCGs tended to absorb the costs, patients incurred costs, or the choice was made for the vaccine not to be administered at all. The consequence is that some patients across England with health needs are not being adequately vaccinated due to confusing funding arrangements, nor is uptake effectively measured. A recent roundtable with immunisation experts identified the need for clearer guidance on the arrangements for dealing with disease outbreaks.133Vaccinating outside Section 7a- immunisation programmes: who, how and why?, British Journal of Healthcare Management, Vol. 25, No. 9 (2019), 275–281 [link] A recent, relevant example is the increase in cases of diphtheria amongst asylum seekers and refugees. UKHSA has issued guidance recommending healthcare staff involved with supporting new arrivals complete immunisations as per the UK schedule.134Felicity Knights, Shazia Munir, Haja Ahmed & Sally Hargreaves, ‘Initial health assessments for newly arrived migrants, refugees, and asylum seekers’, BMJ (28 April 2022) [link]; Jessica Carter, Anushka Mehrotra & Felicity Knights, “We don’t routinely check vaccination background in adults”: a national qualitative study of barriers and facilitators to vaccine delivery and uptake in adult migrants through UK primary care’, BMJ Open, Vol. 12, No. 10 (2022) [link]
Policy Exchange propose that new guidance is issued by NHS England, coupled with a backstop mechanism to address immunisations expected to be provided within clinical care but which do not currently fall under S7a programme delivery.3 Necessary uplifts would be made to the annual vaccines budget to enable providers to be reimbursed. This should be accompanied with greater transparency over the budget for immunisation. Currently, the total Section 7a budget is revealed, but this is often topped-up by NHS England, meaning discrepancies year-on-year in reporting. This will be of increasing importance as the complexity of screening and immunisation programmes increases over time.
Vaccination Collaboratives
Recommendation. NHS England should announce a pilot scheme (in three places) for assessing a singular block contract payment model for vaccination by allowing the development of ‘Vaccination Collaboratives.’
“In any field, improving performance and accountability depends on having a shared goal that unites the interests and activities of all stakeholders. In health care, value is defined as the patient health outcomes achieved per dollar spent. Value should be the preeminent goal in the health care system because it is what ultimately matters “
Michael Porter, Harvard Business School
A central idea in this report is to create a new organisational form to deliver vaccines: the Vaccine Collaborative. We have heard throughout our research that local healthcare organisations want to have greater power and agency to protect their populations in the way that best suits them. The social geography of place is fundamentally important, and service delivery footprints need to match those which make sense to local populations. We have also heard complaints about the current payment system. Central Government suggests that it is distorted towards certain providers, whereas some providers feel the latest set of payment reforms and creation of immunisation as an essential service, are inflexible to geographical and demographic differences between areas.135Caitlin Tilley, ‘Some GP practices face losing up to £66k in child immunisation payments’, Pulse, 5 April 2022 [link]
Evidence also suggests that major reforms from the centre – even when grounded in good evidence and well intentioned – can often lead to unintended consequences. As we described earlier, citizens are sensitive to changes in how they access public services. Moving vaccination delivery from one site to another could be based on convincing pilots or case studies from outside of England – but attempting to roll out a single solution across a population of 60 million people will not work.
Our proposal intends to respond directly to that perspective. We know that the Provider Collaborative model is growing in importance across secondary care (see Box 6), and alongside this we are seeing a movement towards new forms of blended payment. These combine a block element with a gain and risk share element to reflect progress towards objectives. Uncoupling the payment system from raw activity delivered (as is currently done through item of service payments) does carry risks. As we have set out in earlier research, in areas such as elective care there is likely to still be a strong role for payment by results (PbR).136Robert Ede & Sean Phillips, A Wait on your Mind? A realistic proposal for tackling the elective backlog, Policy Exchange, 22 July 2021 [link]
| Box 7. What are Provider Collaboratives? |
| NHS England define provider collaboratives as two or more NHS trusts/foundation trusts working at an appropriate scale across places to join up services.
How we got here: The mental health Vanguard programme in the mid-2010s highlighted the benefits of different providers locally working together to solve problems.137Chris Naylor, Anna Charles & Holly Taggart, Mental health and new models of care, The King’s Fund, 18 May 2017 [link] This led to the emergence of NHS-led provider collaboratives in 2020 – groups of providers in specialised mental health, learning disability and autism services. Some benefits have already been felt. In one example – the Eating Disorder Collaborative in the West Midlands – commitments to share residential capacity meant a dramatic reduction in out-of-area placements, with 34 patients moved back within the footprint in 2021 alone. The money saved has been re-invested in community services.138West Midlands Adult Eating Disorders Provider Collaborative [link] Looking forward: As of July 2022, most NHS trusts are required to be part of a provider collaborative. Broadly these changes sit outside of the legislative proposals in the Health and Care Bill and have therefore attracted little scrutiny. Some researchers have identified possible tension between the role and function of provider collaboratives and the integrated care system architecture. Careful attention will need to be paid to governance, geographical footprints, and culture to ensure that the model is successful.139Charlotte Wickens, Provider collaboratives: explaining their role in system working, The King’s Fund, 21 April 2022 [link] |
The principles for establishing a Vaccine Collaborative would be as follows:
- A group of providers (at least two or more organisations) would come together working at scale across a defined place (circa 250,000 population) with a shared purpose to achieve high vaccine coverage rate and make most efficient use of workforce, and data.
- The Vaccine Collaborative would assume responsibility for delivering all immunisations for the eligible population within that area.
- There would be no restriction on the representation of different partners in the system. We would for example envisage a greater role for local authorities to be involved in the delivery of immunisation alongside the current assurance role. Voluntary sector organisations (e.g., St John Ambulance) could be a local delivery partner.
- The lead provider would need to be a primary care organisation. This would typically comprise a larger GP practice, Federation or Primary Care Network. Further organisations would be sub-contracted. The lead provider would have ultimate responsibility for ensuring sufficient performance indicators are met on coverage and affordability.
- In return, payment for vaccinations and immunisations would be delivered under a new system using capitation, comprising two elements: the first would be a block with two-thirds of the total immunisation budget for that population. Up to one third would be performance related
- Specific targets would be negotiated between NHS England and the Vaccine Collaborative to reflect historic coverage in their patch. Over time, agreed coverage targets would be replaced, assessing health protection performance against a wider set out outcomes.
- A form of automated repayment would be set out in the commissioning intention and contracts, to be used if coverage fell below an agreed level. Including this mechanism rather than relying on clawback would achieve transparency and ensure best value for taxpayer money.
- Providers would be given the autonomy to develop a strategy to meet these targets, with a light touch oversight regime from the centre.
- Leadership of the collaborative would be in the form of a Nominated Immunisation Lead, either an experienced nurse or GP, but could also be the relevant Director of Public Health.
We are confident that this approach would create bold new possibilities for public health. A proposed outline of the Vaccine Collaboratives is shown below, alongside some practical details on how the incentive and organisational form would be designed.
Figure 4 – Vaccine Collaboratives and future of vaccination settings
Commissioning for outcomes: the collaboration model
The separation of commissioning and provision has brought several advantages to the NHS. However, the focus on understanding the value and function of activity, linked to reimbursement, has limitations in health protection programmes such as immunisation.
A focus on activity and output-based metrics has been further reinforced by short term planning and contracting cycles. Contracts with GPs and pharmacists are renegotiated on an annual basis, and by linking income to volume of activity through enhanced services, providers often last the security to make the necessary transformational investments in clinical services.140Tim Ballard, Nicholas Hicks and David Paynton, ‘Outcome-based commissioning: has its time come?’, British Journal of General Practice, Vol. 66, No. 644 (2016), e219-e221 [link] This includes new models of immunisation delivery.
Evidence also suggests that providers are incentivised to deliver better outcomes and achieve greater efficiency when they receive a multi-year contract. Under our proposal, Vaccine Collaboratives would be allocated a multi-year contract (3-5 years) and bring together general practice (working as PCNs), community pharmacy, and other providers, such as SAIS and sexual health clinics (where appropriate), as well as other non-healthcare organisations to use their local assets to collectively meet the immunisation needs of their citizens.
Financial Incentives
A potential challenge over the effectiveness of vaccine collaboratives lies in its incentive structure–– will shifting the incentives away from volumes of jabs administered and towards wider public health outcomes lead to an increase or reduction in coverage? The current vaccine contracting approach (see Box 5 for how GPs are currently reimbursed) is based upon payment per jab administered. Evidence of the effectiveness of financial incentives is mixed. It can drive action in some areas of QOF, but this is not guaranteed.141Rishi Mandavia, Nishchay Mehta, Anne Schilder & Elias Mossialos, ‘Effectiveness of UK provider financial incentives on quality of care: a systematic review’, British Journal of General Practice (2017) Vol. 67, No. 664, e800-e815 [link]
The use of competition-related mechanisms within immunisation has achieved middling returns; areas which have historically struggled with coverage such as London have continued to show limited progress, with ‘vaccine apathy’ a particular challenge in addressing disparities between boroughs.142Daniel Keane, ‘‘Vaccine apathy’ slowing down London’s Covid booster rollout ‘, Evening Standard, 4 November 2022 [link] The current threshold of 80% does not incentivise the services to reach out to underserved population, as it is usually the remaining 10-20% of the population that are traditionally underserved, such as the travelling community, migrant workers, the homeless, or those not registered with a GP143A review of research into vaccine uptake in the UK, Local Government Association [link]. Reaching these populations will require additional resource (as well as services).
The 2021/22 GP contract saw vaccination and immunisation become an essential service with a standardised item of service (IoS) fee set at £10.06 for most vaccines. A graded points system was introduced to incentivise surgeries to reach 95% coverage. These were the most significant reforms to immunisation payments in three decades. They need time to bed-in nationally. However, the broader shift within the system to new, non-activity payment methods should create opportunities for a collaborative approach on vaccination, too. We believe NHS England should announce a pilot for assessing a singular block contract for vaccination. A block contract is a payment framework in which there a fixed budget to a provider to deliver a specific service or intervention.144Models for paying providers of NHS services, BMA, 24 March 2022 [link]
| Box 8 – Protecting the Exchequer Interest Through Clawback |
| We recommend that Vaccines Collaboratives would be paid through the new Aligned Payment and Incentive rules (which feature a fixed element of payment; a variable element (relating to the volume of immunisation activity); and a quality-related element, comprising payment in relation to Best Practice Tariffs and the Commissioning for Quality and Innovation (CQUIN) framework). A significant feature of the contract would be its automatic financial return provisions to ensure value for taxpayer money. Recent studies have indicated that clawback mechanisms can “lead to better earnings quality (reduced re-/misstatements), better pay-for-performance sensitivity, increased firm performance, greater value relevance, and lower overinvestment”.145Patrick Velte, ‘Determinants and consequences of clawback provisions in management compensation contracts: a structured literature review on empirical evidence’, Business Research, Vol. 13 (2020), 1417–1450 [link]
The aim is to enable recipients to develop and provide services over the longer term while securing value for public funds. Such contractual features are not new to the NHS, given it already includes clawback mechanisms in respect of the dental contract, relating to Units of Dental Activity (or UDAs).146Prototype exit arrangements – Dental reform contract transitional guidance: Managing practices and patients in transition, NHS England, 5 April 2022 [link] |
Making it happen
Vaccine Collaboratives are a new concept. It would be unwise to adopt this idea wholesale and to roll it out nationally, immediately. We recommend that instead a period of field testing takes place in the form of a pilot amongst a three ICSs with diverse economic and demographic characteristics––which may consist of:
- 1 ICS in a large city
- 1 rural/coastal ICS
- 1 Town
Getting the first collaboratives structure up and running would take a minimum of twelve months, meaning that the earliest launch date would likely be mid-2024. Amendments may be required to the GMS Statement of Financial Entitlements, and the Community Pharmacy Contractual Framework to allow for the novel payment mechanism.
As outlined in the principles above, in most instances a significant proportion of immunisations in vaccine collaboratives should continue to be led by general practice. We may however see flu and COVID vaccines to be delivered either by a more diverse vaccinator workforce, or for greater volumes to be shifted to alternate provider settings. There may – for instance – be a role for pharmacy to deliver a greater proportion of ‘out of hours’ or weekend immunisations, where GP practices are unable to do so.147Jeffery A. Goad, Michael S. Taitel & Leonard E. Fensterheim et al., ‘Vaccinations Administered During Off-Clinic Hours at a National Community Pharmacy: Implications for Increasing Patient Access and Convenience’, The Annals of Family Medicine, Vol. 11, No. 5 (2013,) 429-436 [link] This is a key starting point for our recommendations.
Spreading Best Practice
Recommendation. DHSC and DLUHC should encourage Health Protection Boards to undertake local stocktakes of their vaccination strategy and performance (in the context of wider health protection provision), to profile disparities and to consider efforts required better meet the needs of underserved communities by Autumn 2023.
As a health system, it is important to document lessons learnt from different approaches to avoid committing the same mistakes. These include systemically overlooking the needs of underserved populations, the failure to address vaccine concerns of certain groups, or poor data infrastructure that prevents effective immunisation surveillance. The sharing of best practice is an effective way of enabling teams to learn and to exchange insights on approaches to vaccination rollouts. The COVID-19 pandemic sped up learning processes with different communities responding in diverse and innovative, ways, these valuable lessons should be heeded and not forgotten. With local government playing a prominent role and DsPHs often playing a convening role between stakeholders to coordinate rollouts, there is particular value in assessing their findings. Some systems have already undertaken such a stocktake. Greater Manchester is one example, resulting in the publication of a recent report from the Independent Inequalities Commission which considers factors affecting the social determinants of health in the round.148The Next Level – Good Lives for All in Greater Manchester, Greater Manchester Independent Inequalities Commission [link]
Whilst there is no shortage of best practice, this is not currently compiled and published routinely at a national level. We propose that a dedicated page should be created (which could be hosted and coordinated by the NIS) by NHS England which brings together existing best practice case studies for immunisation whilst also creating new ones as appropriate drawing upon evidence from CQC, NICE and based upon system level coverage reports. The Playbooks approach from NHSX taken to highlight innovation in elective care may be a useful model to replicate. Most significantly these profiles should highlight processes and steps taken to achieve the outcome – to create a positive learning culture between places and systems. UKHSA’s Vaccine Update is another source of information for end users (e.g., updates to Green Book) which provides another location for providers to review and ensure they are consulting the latest guidance.149Vaccine Update, UKHSA [link]
The role of Integrated Care Systems
Recommendation. The commissioning of immunisation should be delegated to integrated care boards (ICBs) over time. Within this:
- Aligned to the greater role that ICSs will play in enabling the development of ‘Vaccine Collaboratives’, they should be increasingly responsible for the commissioning of ‘evergreen’ immunisation offers, working with local government to develop roving or mobile units, directed toward areas and communities of under-provision or lower uptake.
- Greater support should be earmarked for ‘specialist’ vaccination clinics to improve uptake amongst those with learning disabilities and autism.
ICBs
The new ICS structures should play an enabling role for immunisation, both commissioning and providing oversight to traditional providers and Vaccine Collaboratives where they are established. Expertise for vaccination currently sat within the NHS England Regions is valuable and we would envisage it is gradually redeployed to ICSs as NHS England Regions take on a more strategic role. This must be carefully reviewed however, as precedence has shown that regional commissioning support units (operating on behalf of several CCGs) were able to deliver savings through unifying approaches at this greater, sub-national scale.
Non-traditional providers
Vaccine equity should remain a key priority of the agenda. A notable feature of the COVID-19 vaccination campaign was the greater use of novel settings for vaccination. This brought with it a range of advantages (such as expanding the accessibility of sites, improved community engagement) as well as disadvantages (struggle to ensure good ventilation or the maintenance of cold chain or waste management). Buildings with larger capacities, such as leisure centres enabled higher throughput; the use of religious venues boosted the accessibility of vaccines for some communities. Roving and mobile operating models were also developed to become far more commonplace.150Standard Operating Procedure: Roving and mobile models, NHS England [link] A comparison of delivery site costs is included in Chapter 2.
ICSs should play a central role in expanding ‘evergreen’ immunisation offers for users, utilising non-traditional providers and working with local government, and their public health teams to improve the accessibility and equity of vaccine uptake, especially to those that are systemically excluded from routine immunisation delivery, such as among homelessness people, traveller communities who do not frequently interact with health systems or home-school students who may be left out from primary school-led teenage immunisation programmes. These non-traditional providers could also include greater use of secondary settings, such as children’s hospitals and units with tertiary paediatrics for delivering of (opportunistic) child immunisations, or outreach programmes through mobile clinic (see Box 8) or drive-through clinic (See Box 9).
To achieve this, data quality and sharing must improve to enable this (see Chapter 2.3 on Data), including adaptations to Child Health Information Services (CHIS) so that it can be used in a greater array of settings. Examples in the adult programme would include specialist HIV clinics.
| Box 9. Pop-Up Clinics: Durham County Council |
| Durham County Council delivered mobile pop-up clinics using MELISSA Training provided by Health Education England, collaborating with a range of stakeholders including healthcare providers, local authorities, and the voluntary sector. Twenty-three mobile pop-up services in all were delivered between May and November 2021.
Why Was it Successful? Targeting Underserved Populations The Public Health Intelligence Team mapped Lower Super Output Areas (LSOAs), where vaccination uptake was smaller than 50% to identify areas most in need to support a targeted approach. Certain groups were identified, and the location mapped were designed to accommodate their needs. For instance, they offered mobile pop-up vaccination clinics at Gypsy Roma Traveller temporary stop over sites as well as workplace settings such as Amazon (Bowburn) and the Newton Aycliffe Industrial Estate. Communication and Outreach To engage communities, a social media campaign was undertaken locally, promotional vaccine event leaflets distributed to houses in streets/shop windows identified as low-uptake areas and through communities/businesses via Area Action Partnerships, Welllbeing4Life services, Business Durham and other local stakeholder networks. Outcomes The total number of COVID-19 vaccinations delivered across twenty-three mobile pop-up clinics was 7,988. The majority of those vaccinated were between 18-29, with a higher proportion receiving their first dose, as opposed to 50+ age groups who accessed booster shots via this route (see chart below). Pop-up services significantly increased the rate of vaccination. For instance, Ferryhill’s uptake increased 929% from a 7-day average of 31 doses delivered to 344 doses given in a single day. Cost They calculated the additional cost of the mobile pop-up vaccination clinic to be £5.29 per vaccine. This figure was calculated by dividing total labour costs (excluding staff within the local vaccination services) divided by the number of vaccines given. This is above the cost per dose paid to the provider and the cost of communication resources. Learnings:
|
| Box 10. A Drive-Through Clinic – Derbyshire Community Health Services NHS Trust |

|
Specialist vaccination clinics
Additional resource should also be targeted by ICBs to ensure improved provision of ‘specialist’ vaccination clinics to improve uptake amongst those with learning disabilities and autism. There are roughly 30,000 people with learning disabilities within each of the 42 footprints. Evidence suggests that this cohort are more likely to be fearful of medical procedures – although this trend was less prominent during COVID-19 vaccination. Whilst many will have needs appropriately met in general practice, there are still too many instances of users excluded because of the lack of a tailored approach. Specialist clinics would typically involve minor adaptations to an existing site (which includes GP surgeries) to make it a calmer environment, with longer, staggered appointments and a higher proportion of staff with particular expertise, such as learning disability nurses. Although there are a few successful examples such as the one introduced at James Paget University Hospitals (see Box 10), far too often these services are unavailable. There is a role here for ICSs to identify sites to accommodate the need of a historically underserved and vulnerable population.
| Box 11. An Accessible Vaccination Clinic – James Paget University Hospitals NHS Foundation Trust |
People with learning disabilities and autism (LDA) are underserved in routine programmes and have been disproportionately affected by the Covid-19 pandemic. In 2017-2018, only 44.9% of people with a learning disability received a seasonal flu vaccination.152Creating a Covid-19 vaccination clinic for people with learning disabilities, Nursing Times, 21 June 2021 [link]
How and why it worked
|
Making Better Use of Secondary Care Settings for ‘Opportunistic’ Vaccination
The opportunity to conduct immunisation opportunistically in secondary care settings has long been discussed.154S P Conway, Opportunistic immunisation in hospital, Archives of Disease in Childhood, Vol. 81, No. 5 [link] Many hospitals deliver the neonatal immunisation schedule due at 8, 12, and 16 weeks for at-risk infants, but secondary care settings are not routinely utilised for immunisation. There are good reasons for this. Vaccination may take away valuable time from a workforce focused upon specialised care; the ‘opportunistic’ nature of immunisation may not allow for ‘economies of scale’ incurring higher costs (procurement, cold chain facilities etc.) where a dedicated clinic (and often, a dedicated nursing workforce) needs to be established. There is also the ‘cognitive load’ of patients and their families to bear in mind – would immunisation just become another thing to consider when users are in hospital to address more acute health issues? As such, we are of the view that the use of secondary settings should only be supplementary to the use of primary care settings for vaccination.
Whilst it is neither feasible, nor desirable for immunisation to be introduced across all care settings, there are however particular opportunities which ought to be explored further. Our view is that the Government should undertake a comprehensive review exploring the possibilities for vaccination outside of primary care settings, assessing its effectiveness in driving uptake and in delivering value for taxpayer money.
There is a body of evidence which demonstrates the benefit of enabling ‘opportunistic’ vaccination in secondary care settings, with studies finding acceptability amongst users and clinicians.155I.Plumptre, T.Tolppa & M.Blair, ‘Parent and staff attitudes towards in-hospital opportunistic vaccination’, Public Health, Vol. 182 (May 2020), 39-44 [link]; I.Plumptre, T.Tolppa & M.Blair, ‘G431(P) An audit of vaccination adherence and acceptability of opportunistic vaccination in inpatient paediatrics’, Archives of Disease in Childhood, Vol. 103, Issue Supplement 1 (2018) [link] A recent study from the United States showed that even modest increases in the screening rate for influenza vaccine status amongst hospitalised patients with asthma resulted in clinically significant increases in those fully immunised.156Ronald J. Teufel, William T. Basco Jr. & Kit N. Simpson, ‘Cost effectiveness of an inpatient influenza immunization assessment and delivery program for children with asthma’, Journal of Hospital Medicine, Vol. 3, No. 2 (2008), 134-141 [link] Both emergency and tertiary paediatric units can play a useful role in identifying under-immunised children and facilitate catch-up immunisations, where effective information systems are in place.157Simon Shingler, Kim Hunter, Andrina Romano & David Graham, ‘Opportunities taken: The need for and effectiveness of secondary care opportunistic immunisation’, Journal of Paediatrics and Child Health, Vol. 48, No. 3 (2012), 242-246 [link]; Bahar Behrouzi, Deepak L. Bhatt & Christopher P. Cannon et al., ‘Association of Influenza Vaccination With Cardiovascular Risk: A Meta-analysis’, JAMA Network Open, Vol. 5, No. 4 (2022) [link] Some hospitals – such as Chelsea and Westminster – can check immunisation status during A&E triage enabling this already, but this is not commonplace. One of Manchester’s largest trusts is currently piloting a scheme whereby a dedicated immunisation team works alongside midwives to support vaccination. The findings of the pilot will be revealed in Summer 2023 and could be instructive for approaches taken elsewhere.
There is also evidence to suggest that parents who decline immunisation for their children in the community may agree to vaccination in hospital.158 Ingrid Berling, Jody Stephenson & Patrick Cashman, ‘Opportunistic childhood vaccinations in emergency—Are we really missing anyone?’, Australasian Emergency Care, Vol. 15, No. 1 (2012) [link] Through effective collaboration with inpatient clinical teams, opportunistic immunisation can be achieved.159Sonja Elia, Kirsten Perrett & Fiona Newall, ‘Providing opportunistic immunisations for at-risk inpatients in a tertiary paediatric hospital’, Journal for Specialists in Paediatric Nursing, Vol. 22, No. 1 (2017) [link] For individuals with chronic diseases more susceptible to vaccine-preventable diseases and have an increased risk of associated disease severity and complications, there may also be opportunities to boost the opportunistic vaccination offer in a targeted manner.
However, to realise benefits here, investment in staff training, education and support will be required. It will be crucial to evaluate whether this offer would be optimal and cost-effective. Moreover, information systems and data sharing require significant improvement. A 2021 study conducted in Greater Manchester showed that once vaccination data left primary care, it passed through 1 of 10 local child health information services (CHISs), using an assortment of different information technology systems, after which it shed individual identifiers and was aggregated within national systems. None of the existing CHISs in Greater Manchester were accessible to those working in the paediatric emergency department.160Rachel Isba, Nigel Davies & Jo Knight, ‘Are child health information services a viable source of accurate vaccination data for clinicians working in paediatric emergency departments in England?’, BMJ Health and Care Informatics, Vol. 28, No. 1 (2021) [link] These findings align with those we set out in Chapter 3, section entitled ’Data’.
3.2. Workforce
“The aim must surely be to create the conditions where healthcare professionals are doing the tasks that ‘only they can do’ or that they are best-placed to carry them out”
Semi-structured interview, 2022.
Recommendation. The upcoming 15-year workforce strategy being developed by Health Education England should make a series of recommendations on the optimal workforce for vaccination. This will require joint working including with local government, the VCSE sector and the Royal Colleges, but is likely to involve the introduction of more diverse workforce for the administration of vaccines, with GPs and nurses (the latter of whom currently deliver the bulk of vaccinations) increasingly adopting a supervisory roles. Developments could include enabling all nursing, medical and pharmacy students to opt-in to deliver seasonal vaccinations, where adequate clinical supervision can be assured, with NHS England introducing contractual arrangements and indemnity to enable it.5
Recommendation. ‘Neighbourhood Immunisation Coordinators’ should be established as part of Integrated Neighbourhood Teams as proposed by the Fuller Review.
Recommendation. Adaptions to the National Protocol and National Patient Group Direction (PGD) mechanisms to maximise the vaccination workforce, where it can be done so safely should be introduced. This would include:
- The use of national protocols, such as Regulation 2 of the NHS Regulations 2013 removing the requirement for those administrating COVID vaccines to be registered on the medical performers list where it is clinically appropriate to do so.
- Pharmacy Technicians should be added to the list of those able deliver vaccines through a Patient Group Directive (PGD) with an amendment to The Human Medicines Regulations 2012.
It is widely known that the UK faces pressing workforce shortages in health and care, with 39,000 unfilled nursing posts – for instance – equating to a vacancy rate of 10% (as of March 2022).161Denis Campbell, ‘Staffing crisis deepens in NHS England with 110,000 posts unfilled’, The Guardian, 3 March 2022 [link] The rate-limiting factor in expanding the provision of services – across primary and community care in particular – will be predicated on approaches which can boost the workforce overall. This necessitates an approach which strengthens the role of the primary care and public health workforce, with a need to focus upon growing the number of GPs, nurses and pharmacists who deliver the bulk of vaccinations. In the short to medium term however, a team-based approach to maximise skill mix in immunisation should be adopted as a pragmatic approach to maximise existing talents and to create opportunities to boost the overall workforce.
We therefore identify three approaches to create more capacity for vaccination:
- By focusing upon increasing the overall number of qualified healthcare professionals;
- Distribution of tasks more efficiently within the existing and emerging workforce to free-up time through delegation (team-based skill mix). Medical and nursing students, retired health workers and care home staff are all professionals who should be considered in future immunisation workforce plans developed at both local, ICS and national levels.
- Train a non-clinical ‘surge’ workforce that can be deployed when there is a need to vaccinate in large numbers on a seasonal or temporary basis (resilience).
However, there will be limits to this expansion. Those who advise on and/or administer vaccines need to be knowledgeable and skilled. They need to be able to answer patients’ and parents’ questions confidently and accurately, and to explain why vaccines are needed, while dispelling any myths or concerns that may arise.162Helen Donovan & Laura Craig, ‘Why immunisation training matters’, Primary Health Care, 17 July 2018 [link] Considering the unique characteristics and needs of each programme in turn, it is clear that elements of the routine schedule, such as childhood immunisation in particular, require the expert, wrap-around care that is provided in general practice, most often by practice nurses.
Table 10. International Best Practice: Who administers vaccines?
| GPs and Nurses | Portugal, Israel, Sweden and Australia all use doctors and nurses to administer vaccines both during ‘peace-time’ and surge periods. In Sweden, the members of the workforce prior to the pandemic deemed suitable to administer vaccines included physicians and nurses only. |
| Pharmacists | In Australia, Portugal, Switzerland, Israel, and the UK, pharmacists administered vaccines in addition to physicians and nurses. |
| Paramedics, medical students | In Israel, while most immunisers are nurses, the government quickly changed its regulations to allow practice medics and paramedics to administer vaccines165. |
| Volunteers | Legislation was amended to allow a wider group of healthcare professionals to administer vaccines (such as physiotherapists) across England. 26,500 clinical volunteers were recruited and trained by St John Ambulance.163Annual report 2021, St John Ambulance [link] |
| Without PSD/medical practitioner’s prescription | In Australia, nurses, pharmacists and midwives can administer routine immunisation without a medical practitioner’s prescription in certain cases: nurses can administer standard immunisation schedule; pharmacists can administer Influenza, MMR, dTp, and Meningococcal ACWY vaccines; Midwives can administer Pertussis and Influenza vaccines164.
Israel also authorised nurses during the pandemic to independently assess which individuals meet the clinical criteria for vaccination without requiring consultation with a physician. |
| Non-clinical | In Israel, supplementary non-clinical staff were recruited from the Home Front Command of the Israel Defence Forces (IDF).
The UK recruited non-clinical volunteers through the national NHS Volunteer Responders programme |
Developing Specialists and Supervisors
Nursing is under-resourced across primary and community settings at present, with knock-on effects for the development of an experienced workforce to support immunisation at neighbourhood level.164Julia Taylor, ‘Why nursing is so important in tackling current challenges in primary care’, Nursing in Practice, 26 August 2022 [link] The concept – first discussed in the Briggs Review of 1972 – that we must make “best use of available manpower”, still stands and should guide the future approach.165Report of the Briggs Committee on Nursing, October 1972 [link] We believe that GPs and experienced nursing professionals should increasingly undertake clinical supervision and leadership roles (including as immunisation leads in vaccine collaboratives). We know that working toward specialist or advanced skills can positively motivate the workforce and can help with retention. This applies to the entire workforce. For those training as Advanced Nurse Practitioners (ANPs) for instance, where it can be common for individuals to move, once qualified, unless new responsibilities are encouraged, expanding their role in vaccination is one route that ought to be considered.166Jennifer Aston, ‘The future of nursing in primary care’, British Journal of General Practice, Vol. 68, No. 672 (2018), 312–31 [link]
Given the decline in recent years in the number of health visitors, opportunities to develop the crucial role these professionals play in developing vaccine confidence amongst new parents, should also be leveraged.167Bethany Boddy, ‘Newly qualified health visitor: Discussing vaccinations with families through health visiting contacts’, Journal of Health Visiting, Vol. 7, No. 10 (2019) [link]
| Box 12. Case study: Scotland’s Vaccination Transformation Programme |
| Since 2018 in Scotland, GP practices no longer provide vaccinations under their core contract as enhanced services. Instead, NHS boards have set up and staffed community vaccination centres—many operating from NHS board-owned health centres168‘Scotland to get national vaccines service’, Healthandscare.scot,19 April 2022 [link] .
Upon implementation, the biggest challenge faced was to deliver the annual adult flu vaccination programme requiring over 70% of doses to be delivered in a two-month period. The NHS Boards explored the use of Health Care Support Workers (HCSWs), as part of their local teams to ease the pressure on the existing workforce during the winter surge months169Letter from Deputy Chief Nursing Officer Designate re. National Framework for Vaccine Administration by Healthcare Support Workers in Scotland V2.0 (July 2021), 30 August 2021 [link]. HCSWs were already being used to support the delivery of Flu and COVID-19 vaccines during the pandemic. Changes to the Human Medicines Regulations brought a new regulation (247A) permitting the supply or administration of a medicinal product used for vaccination or immunisation against coronavirus or influenza by a specified class of people, which need not be limited to registered healthcare professionals, including HCSWs.170Letter from Deputy Chief Nursing Officer Designate re. National Framework for Vaccine Administration by Healthcare Support Workers in Scotland V2.0 (July 2021), 30 August 2021 [link] Those that are permitted to vaccinate under the National Protocols for Flu and COVID-19 and considered as Health Care Support Workers includes:
Consistent with our own proposals, the measures do not support HCSWs administering vaccines to pre-school age children, to administer other live attenuated vaccines as part of a re-immunisation or booster programmes following disease or treatment or to administer Travel Vaccinations. |
‘Neighbourhood Immunisation Coordinators’ should be established and linked to ‘Integrated Neighbourhood Teams’, proposed by the Fuller Review. These would be named individuals who can respond to queries and provide a local focal point. The role would typically be filled by a clinician or public health expert, although that is not a requirement. It would be the equivalent of 0.25 whole time equivalent role, paid at AfC band 8a. Concurrent with most recent NICE guidelines, this could overlap with the nominated person responsible for identifying housebound immunisers.171Vaccine uptake in the general population, National Institute for Health and Care Excellence, Guideline NG218, 17 May 2022 [link]
Expanding the public health (and wider health protection) workforce
There is a need – as it was put to us – to “democratise health protection skills”. This is a view which accords with the findings of the RSPHs recent ‘Rethinking the Public Health Workforce’ report, which sets out the need to raise the profile and expand opportunities to play a role in public health protection.172Rethinking the Public Health Workforce, Royal Society for Public Health [link] Greater uptake therefore of RSPH qualifications should be encouraged, whilst NHS England should work to clarify medical indemnity for the non-clinical workforce to support vaccination.
Student Nurses & Medical Students
There is also an opportunity to boost the vaccination workforce by offering greater opportunities to medical and nursing students. During the pandemic, the national protocol provided a vehicle for supervised student nurse placements within mass vaccination centres. A study of one such placement in South Wales for undergraduate pre-registration student nurses concluded that a placement within a mass vaccination centre offered “a rich educational experience for student nurses, which as yet appears to be underutilised across the UK”.173Matthew Thornton, Linda Jones, Rhiannon Jones, Gail Lusardi, ‘If the public can vaccinate, why not students? Review of a student nurse placement in a mass vaccination centre’, British Journal of Nursing, Vol. 31, No. 7 (2022) [link]
Policy Exchange believe students should be offered the possibility to opt-in to deliver high-volume, or seasonal jabs, such as influenza and COVID-19 under the professional direction of registered health care professionals. Students should not take on any vaccine-related role if already on placements and contracts should be arranged to ensure roles are formalised so they can operate as employees and can be indemnified under the Clinical Negligence Scheme for General Practice (CNSGP), as the British Medical Association have advocated.174COVID-19 vaccination programme: extra workforce, BMA, 14 February 2022 [link] A new minimum expectation would be to encourage students to support with vaccine deployments for at least two days over the course of their studies– except where there is a strong clinical rationale for not doing so (or adequate supervision cannot be assured).
Vaccination as a route into (and back into) the NHS
Efforts to leverage the attractiveness of vaccination activity should encourage the development of dedicated schemes developed by ICSs to enable nurses and GPs – either those who have recently retired or who may have taken a career break – to undertake vaccination as a specific, protected activity. The many thousands of nurses who have lapsed nursing registrations might be attracted back to the workforce by completing a nationally funded Return to Nursing course and could be encouraged to undertake roles delivering vaccine clinics specifically – this is an approach that Policy Exchange proposed in a recent report.175Robert Ede, Sean Phillips & Yu Lin Chou, ‘What do we want from the next prime minister? Health and social care’, Policy Exchange (August 2022) [link]
Concurrent with our view of the need to broaden the health protection workforce overall, there also needs to be a greater focus on creating pathways for the current non-clinical and volunteers to further enhance their skills and experience – with the creation of dedicated routes to becoming specialist immunisers with further training.
The Value of Volunteers
A clear positive of the pandemic was the growth of a volunteer workforce across the NHS. It has led Wes Streeting MP, Shadow Secretary of State for Health and Social Care to express an interest in the development of a “standing jabs army” to support future vaccination efforts.176Quoted during ‘In conversation with Wes Streeting MP, Shadow Secretary of State for Health and Social Care’, Institute for Government, 7 June 2022 [link]; reiterated since in Lizzie Roberts, ‘Bring in the ‘Jabs Army’ to fix NHS blood service staffing crisis, says Wes Streeting’, Daily Telegraph, 16 October 2022 [link] NHS Professionals recruited and trained thousands of volunteers to administer Covid-19 vaccines177NHS Professionals [link] 26,500 clinical volunteers were recruited by St John Ambulance in 14 weeks working as patient advocates, care volunteers and vaccinators; 92,000 non-clinical volunteers were recruited through the national NHS Volunteer Responders programme.178The rollout of the COVID-19 vaccination programme in England, National Audit Office, 25 February 2022 [link] Indeed, 11,483 volunteer vaccinators, introduced during the pandemic have since decided to start a new career in the NHS, with some studying for clinical roles or others taking up jobs supporting medical teams. There is therefore a longer-term benefit with the possibility to create permanent employment pathways for volunteers.179Nicola Davis, ‘More than 11,000 decide to join NHS after being Covid jab volunteers’, The Guardian, 18 April 2022 [link]. It is important that a distinction is made however between a workforce flexed for ‘surge’ periods and that operating ‘in peacetime’. Whilst it is crucial to maintain a reservist volunteer workforce that can be rapidly scaled up in situations of a pandemic or during seasonal flu campaigns, it is important to have long-term workforce dedicate to delivering immunisation programmes in normal time. Training is often a significant burden on existing, qualified staff, particularly for those operating in sites with high proportions of temporary and bank staff.180A recent analysis of six seasons of the childhood influenza national vaccination programme is instructive: George Kassianos, Pauline MacDonald, Ivan Aloysius, Arlene Reynolds, ‘Implementation of the United Kingdom’s childhood influenza national vaccination programme: A review of clinical impact and lessons learned over six influenza seasons’, Vaccine, Vol. 38, No. 36 (2020), 5747-5758 [link]
Regulatory Reform & National Protocols
A shift enabling an expansion of those able to vaccinate has been supported by pragmatic changes to national protocols, to enable – where appropriate –non-clinicians to administer vaccines. Regulation 2 of the NHS (Performers Lists) Regulations 2013 removed the requirement for those administering COVID vaccines to be registered on the medical performers list – a move which should be maintained where it is clinically appropriate to do so. Volunteers meeting the criteria in protocols for ‘required characteristics of persons’ administering the COVID-19 vaccine meanwhile were eligible for indemnity under the CNSGP. Exceptions included volunteers who are deployed through the arrangements established centrally by NHS England with St John Ambulance and those in non-clinical roles. We are of the view that nationally procured volunteer contracts should remain in place and should be ‘maximised,’ with ‘reservists’ used across for seasonal programmes such as influenza and COVID-19, enabled by the extension of national protocols.
It remains moreover that in most instances, a Patient Specific Direction (PSD), or a written instruction signed by a prescriber for medicines to be administered to a named patient is required to vaccinate. Whilst there will be a limit to those we ought to include on the list, proportionate reform could bring substantial benefit. Many (although not all) pharmacy technicians are registered healthcare professionals with NVQ level 3 training (those who have trained since the formation of the mandatory register in 2011 certainly will) and have already played an important role in establishing pharmacy-based vaccination centres across England. Current legislation limits their potential in supporting the national drive to vaccinate the population and ought to be reviewed.181Emily Stearn, ‘Government urged to let pharmacy technicians give COVID jabs under PGD’, Chemist & Druggist, 14 Dec 2021 [link]
3.3. Data
“The current system is ‘19th century’––from both the user and public health worker perspective… it is difficult to extract useful data to aid decision-making… often reporting is delayed and systems fragmented”.
Semi-structured interview, 2022.
‘A Single Version of the Truth’
Recommendation. DHSC and NHS England should create a comprehensive immunisation information system (IIS) to modernise immunisation data collection and analysis, drawing upon international best practice, so that everyone works from a ‘single version of the truth.’ This should integrate UKHSA surveillance systems as well as databases held by the MHRA and NIHR.
The experience of COVID-19 shows how data could save lives, and it underpinned the success of a ‘world beating’ rollout in its early stages.182Jennifer Beam Dowd, ‘The UK’s covid-19 data collection has been “world beating”—let’s not throw it away’, BMJ, 25 February 2022 [link] It informed decisions, such as (counterintuitively) halving the supply of vaccines for the Northeast and Yorkshire region to enable poorer performing parts of the country to catch up.183Robert Ede & Sean Phillips, ‘Closing the Covid-19 data gap: Assessing the initial phase of the vaccine rollout’, Policy Exchange, 26 January 2021 [link] In March 2020 meanwhile, the Secretary of State issued NHS Digital with a Control of Patient Information (or COPI) notice, enabling the sharing of confidential patient information. After two years (and three extensions), the COPI notice expired on 30 June 2022. Whilst controversial, COPI enabled the capture of data at a more granular level, including by ethnicity which enabled a greater awareness of disparities and targeted interventions to be developed.
Whilst strides have been made in the past two years revealing the importance of high-quality real-time data for campaigns, and raising the bar as a result, the overall data architecture to support routine immunisations requires significant reform if it is to support a National Immunisation Service, or ‘vaccine collaboratives’ where data sharing between providers would be a significant factor in determining success. There is – as one interviewee put it to us – an enormous “technical debt” to sort. Many issues with immunisation data are long-standing. Building upon proposals in the recent Goldacre Review, investment in embedding data analytical capabilities throughout the system – and particularly at ICS level will be required. A tender for a Federated Data Platform was recently launched, with immunisation included as one of five main functionalities.184It is worth noting the tender has been recently been delayed: Nick Carding, ‘New covid-inspired data system delayed by NHS England’, Health Service Journal, 12 August 2022 [link] Such a platform, if effectively introduced, could potentially integrate existing GP patient records, to allow for population cohorts and vaccine coverage reporting.
By creating an overarching, effective data model, the experience of vaccination for the workforce and users alike can be improved. Indeed, making progress on this agenda will be the high-impact enabler of an improved service overall. But defining the model will be key, such as being deliberate about the choice of indicators; being clear on their definitions, limitations, and methods of measurement; and describing how those indicators work together to give a more comprehensive and practical understanding of immunisation data quality, usability, and use, should yield more informed, and therefore better, programmatic decision-making.”185Peter Bloland & Adam MacNeil, ‘Defining & assessing the quality, usability, and utilization of immunization data’, BMC Public Health, Vol. 19, No. 380 (2019) [link]
The Key Functions of an Immunisation Information System (IIS)186Designing and implementing an immunisation information system: A handbook for those involved in the design, implementation or management of immunisation information systems, ECDC, November 2018 [link]:
- Helps guide decision-making: Evidence-based monitoring of vaccine coverage facilitates decision-making at a population level, such as identifying risk of infectious diseases to plan targeted interventions. Allows evaluation of performance and cost effectiveness.
- Monitors vaccine efficacy: Monitoring of epidemiological impacts corresponding with other data sets held, including secondary-use cases for research.
- Helps reveal health inequity: When an IIS is linked with geographic and socioeconomic characteristics, underserved populations can be identified.
- Empowers users: Enable users to make informed decisions; support the workforce to make clinical decisions on vaccine indications and contraindications.
- Consolidates fragmented records: IIS enables fragmented immunisation records of people immunised across multiple healthcare providers across the life course. This enables healthcare providers to offer a tailored service, such as providing missed vaccinations, and can assist in avoiding errors such as double administration
- Enhances Call/Recall: An effective IIS should enable timely and accurate call/recall notifications.187Peter G. Szilagi, Christina S.Albertin & Alison W.Saville, ‘Effect of State Immunization Information System Based Reminder/Recall for Influenza Vaccinations: A Randomized Trial of Autodialer, Text, and Mailed Messages’, The Journal of Pediatrics, Vol. 221 (June 2020), 123-131 [link]
- Assists in vaccine supply and stock management: can support provider inventories and vaccines reimbursement management
Immunisation Data Systems Used in England Today
The current immunisation information system used across England for immunisations, whilst comprehensive, suffers from fragmentation and inefficiency. Fig. 5 depicts the current system.
The full list of systems currently includes:
- GP registers – GP IT suppliers
- Child Health Information Systems (CHISs) – an NHS-commissioned service responsible for health data for children aged 0-19 in a specified area, into a single child health record. CHIS works with maternity units, general practice, health visitors, school nurses and local authorities
- NHS Digital’s Childhood Vaccination Statistics – by local authority, region and devolved nation188Childhood Vaccination Coverage Statistics, NHS Digital [link];
- The National Immunisation Management System (NIMS) – for Covid-19 and flu vaccination data189National Vaccination Programmes, NHS England [link]
- ImmForm – an UKSHA website used to both collect data on vaccine uptake for the national immunisation programme, and provide ordering facilities for vaccines used in the national immunisation programme
The UK has the longest running population-based child health registers in Europe. Data is currently recorded on two systems: GP registers and population-based child health information systems (CHISs). CHISs are used to estimate vaccine coverage for the routine childhood immunisation programme, which supplies the statistics used in the ‘cover of vaccination evaluated rapidly,’ or COVER programme. GP registers are used to evaluate vaccination programmes for adults (e.g., influenza or pneumococcal).190G Amirthalingam, J White & M Ramsay, ‘Measuring childhood vaccine coverage in England: the role of Child Health Information Systems’, Eurosurveillance, Vol. 17, No. 16 (2012) [link] COVER can be useful during an outbreak of a disease for which some children may not be immunised and provide a population-perspective for all public health programmes.
CHIS, managed by the Child Health Departments in local areas and commissioned by NHSE as part of the Section 7A, hold data of all children living within a local authority. There are many providers, and indeed, the issue of interoperability between local CHISs has long been an issue.191Rachel Isba, Nigel Davies & Jo Knight, ‘Are child health information services a viable source of accurate vaccination data for clinicians working in paediatric emergency departments in England?, BMJ Health and Care Informatics, Vol. 28, No. 1 (2021) [link]
When a child is born, midwives register new-borns on the Central Issuing Services (CIS), which provides information to maternity clinics and local CHISs. CHIS and GPs exchange consent, clinical lists, attendance and notifications. It supports call and recall to parents to remind them of due vaccination.
GPs have their own registers that are operated by commissioned IT providers, where GPs manually input immunisation record unto the system, and then these immunisation data are uploaded automatically to CHIS, for pre-school children, or ImmForm, for those of school-age and adults, depending on the immunisation programmes.
SAIS and health visitors, commissioned by NHSE on the other hand, do not have their own registry, but require the vaccinators to manually input immunisation record directly into the ImmForm system, a secured, Excel database managed by UKHSA. Similarly, hospitals (and pharmacies to a lesser extent, who are commissioned to provide immunisations also input immunisation record manually to the ImmForm system. This process can take up to 18 months causing significant delay for immunisation surveillance. Childhood immunisation data sources from various providers and IT system are then submitted their data to UKHSA for quarterly or annual collection within the agreed deadlines to compile the quarterly COVER or annual reports, after being validated by Strategic Data Collection Services (SDCS).
Table 11. Evaluation of England’s Immunisation Information System
| Functions | Performance | Where/which system |
| Guide decision making (uptake statistics) | Data reporting is not frequent enough to enable local decision-makers to prepare timely interventions, with some childhood immunisation having as much as 18 months lag in reporting. | COVER |
| Evaluate vaccine effectiveness; safety | Often focus on activity-based data (output) and less on outcomes or impact. | NHS Data analytics |
| Detect health inequity | GP has data of their own practice areas, but not shared across settings. LAs and Director of Public Health do not have direct access to CHIS, which is hard to target under-vaccinated areas. | CHIS |
| Consolidate records across health providers
|
Immunisation systems highly fragmented across settings, in part due to a devolved approach to health services | GP IT Providers, CHIS, ImmForm
|
| Consumer’s digital access to immunisation record | Currently only Covid-19 vaccination is accessible online through the NHS App and NHS Portal | Not available in the UK, except for COVID-19 vaccine |
| Call/Recall | Inconsistent reporting through CHIS due to incomplete and delay reporting of immunisation activities192Kerry Lonergan, Ali Latif & Thomas Beaney et al., ‘Implementing the evidence: Are call/recall systems for immunisations feasible in general practice?’, Vaccines and Immunology, Vol. 1, No. 1 (2018), 1-15 [link] | CHIS |
Data sharing and inter-operability
The greatest impediment to cooperative working across primary care providers at present is an inability to seamlessly share data across settings. As part of our research, this has been a consistent and near-universal complaint from those on the front line. We have heard of instances of pharmacies lacking access to school cohort lists required for childhood influenza vaccination; GP practices meanwhile – who have the responsibility for holding a full record of immunisation for those on their patient lists – can be left with incomplete or inaccurate information transfer from other settings, which creates its own ‘failure demand,’ with users incorrectly called (or recalled) for vaccination or teams having to conduct additional work to retrospectively amend information they have received.
Table 12 – Overview of immunisation data collection and systems in England
| Provider | Population | Data system(s) |
| GP practices | Pre-school, adolescent, and adult immunisation programmes, | GP level data uploaded via GP IT suppliers and data linkage systems, such as QMS and Health Intelligence commissioned by NHSE, to either CHIS (0-19 years) or ImmForm. |
| Schools | School-aged immunisation | School-level data inputted to CHIS |
| Pharmacies | Adult immunisation, COVID and flu vaccines | Contractors use a paper-based National Flu Vaccination Record Form when IT support is not available193Flu Vaccination – consent, record keeping and data requirements, Pharmaceutical Services Negotiating Committee [link] . |
| Hospitals | Pre-school, adolescent, and adult immunisation programmes for certain population** | CHIS (0-19 years), ImmForm |
As Table 11 and Fig. 5 suggest, the current data collection system for immunisation data is complex and fragmented. The Covid-19 pandemic, however, has demonstrated the possibility and importance of having an effective, nation-wide data platform: recorded real time, incorporating the whole population, and identifying geographical and demographic characteristics to allow for targeted interventions, through the National Immunisation Management System (NIMS). A recent NAO report found that NHS England and Digital had “created new digital tools to support the vaccine deployment, making effective use of imperfect existing data”.194The rollout of the COVID-19 vaccination programme in England, National Audit Office, 25 February 2022 [link]
Fig. 5 – Data Architecture for Routine Immunisation Programmes
Fig. 6 – Data Architecture Introduced to Manage COVID-19 Vaccination
| Box 13. Israel: A National Immunisation Registry |
| In 2008, the Ministry of Health launched a national immunisation registry based on immunisation reporting from well-baby clinics and school health services. The registry includes all routine childhood vaccinations, incorporating data on vaccine doses and dates, characteristics of children and socioeconomic information. The system is based on registering each child individually during an initial clinic visit, using entries extracted from the national population demographic database to ensure unique automatic identification of the child to prevent database entry errors.
Impact The registry was used to identify measles outbreaks in 2018 and 2019 – in which 2200 cases occurred among ultraorthodox communities in Jerusalem. An outbreak control programme detected unvaccinated children. The campaign led to increased MMR1 coverage rates from 80% to 95% within 3 months.195Chen Stein-Zamir, Avi Israeli & Itamar Grotto, ‘Immunization registry as a digital assessment tool during outbreaks’, Clinical Microbiology and Infection, Vol. 27, No. 2 (2021), P166-168 [link] |
NIMS served as the main system of record for all flu and Covid vaccination programmes across England and holds a near real-time record for all vaccinations given at the individual patient level and scheduled the calling of patients by priority groups via letters, emails, or SMS messages, which is matched to the availability of vaccines. It incorporated a data capture service, collecting information at the point of vaccination including citizens’ demographics, clinical records and vaccination status to integrate with a myriad of other NHS point of care, booking and analytical systems to send and receive data for cohort selection, planning and prioritisation. NIMS provides data to UKHSA and NHSE for analysis and statistics as well as receiving information about vaccinations from GP Practices, pharmacies and other vaccination centres, which allows for information to flow between different settings. A recent review found that NIMS “reduced the risk of inaccurate immunisation records for the entire population” with its point of care apps providing “a more consistent template of entering data”.196Elise Tessier, Julia Stowe & Camille Tsang et al., ‘Monitoring the COVID-19 immunisation programme through a National Immunisation Management System – England’s experience’, accessible via MedRxiv, 22 September 2021 [pre-print] [link] It also helped embed a positive feedback loop for vaccine manufacturers and the life sciences sector, with Public Health England linking testing data to NIMS.197Jamie Lopez Bernal, Nick Andrews & Charlotte Gower et al., ‘Effectiveness of the Pfizer-BioNTech and Oxford-AstraZeneca vaccines on covid-19 related symptoms, hospital admissions, and mortality in older adults in England: test negative case-control’, BMJ, 13 May 2021 [link]
Direct care
A novel approach is required to ensure that all relevant providers can view, amend and update their patient’s immunisation status.198The future of primary care: Creating teams for tomorrow, National Association of Primary Care [link] For instance, health visitors should be able to access to the medical records of the babies and children they are supporting, so they can easily check vaccination status and encourage uptake if appointments have been missed. Pharmacists too – who we envisage are commissioned to deliver a wider range of vaccinations in the future – should be able to view the immunisation record of users to enable ‘opportunistic’ vaccination. Ensuring this information is up to date is key. After all, the Covid-19 vaccination rollout highlighted the importance of accurate medical records for producing reliable lists of people who are clinically extremely vulnerable (CEV), or immunocompromised.199Simon Hodes & Azeem Majeed, ‘Covid-19 vaccines: patients left confused over rollout of third primary doses’, The BMJ Opinion, 15 October 2021 [link]. On learning disability registers, see Lara Shemtob, Rathy Ramanathan & Ken Courtenay, ‘Learning disability registers: known unknowns and unknown unknowns’, British Journal of General Practice, Vol. 71, No. 705 (2021), 153-154 [link]
At the other end of the telescope, there is substantial scope to improve immunisation surveillance. This points to the benefits associated from having a National ‘Life Course’ Registry – a confidential, population-based database that records all immunisation doses administered by relevant providers.200On their international value and use, see Samantha B. Dolan, Emily Carnahan & Jessica C. Shearer, ‘Redefining vaccination coverage and timeliness measures using electronic immunization registry data in low- and middle-income countries’, Vaccine, Vol. 37, No. 13 (2019), 1859–1867 [link] Evidence shows they enable a more robust and systematic approach to immunisation.201Ulrike Baum, Jonas Sundman & Susanna Jääskeläinen, ‘Establishing and maintaining the National Vaccination Register in Finland’, Eurosurveillance, Vol. 22, No. 17 (2017) [link] Some countries with successful programmes – such as Israel, Australia and Sweden– have only introduced these registers in the past five years (see Box 10 & 11).202On the Australian model see: Brynley P. Hull, Shelley L. Deeks & Peter B. McIntyre et al, ‘The Australian Childhood Immunisation Register—A model for universal immunisation registers?’, Vaccine, Vol. 27, No. 37 (2009), 5054-5060 [link]. For a recent assessment, see Lauren G Dalton, Kelley N. Meder & Frank H Beard et al., ‘How accurately does the Australian Immunisation Register identify children overdue for vaccine doses? A national cross-sectional study’, Australian Government Department of Health, Vol. 46 (2022) [link]. On the impact of COVID on AIR, see Jane Tuckerman, Christopher C Blyth, Frank H Beard & Margie H. Danchin, ‘COVID-19 and changes in the National Immunisation Program: a unique opportunity to optimise the Australian Immunisation Register (AIR), Medical Journal of Australia, 5 April 2021 [link].
Secondary uses
The Covid-19 RECOVERY trial was largely dependent on cross-organisational data sharing which gave researchers improved access to primary care data that “would have been difficult to obtain without the COPI notices”.203Hannah Crouch, ‘What does the end of COPI mean for digital health innovation?’, Digital Health, 23 June 2022 [link] Current legislation provides for sharing only for the purpose of direct care. The Government has acknowledged the need to address these challenges. The Data Saves Lives strategy was published in June 2022, arriving hot on the heels of the Goldacre Review.204Ben Goldacre, ‘Better, Broader, Safer: Using Health Data for Research and Analysis (April 2022) [link] Immunisation will be one of five focus areas for an ‘NHS Federated Data Platform’, meanwhile.205‘NHS Federated Data Platform’, gov.uk [link] These initiatives could transform the secondary use of data for planning and research to improve services.
There is an important consumer dimension to these developments. Immunisation data – at a national as well as at a local level – should be transparent, publicly accessible, and updated at appropriate, regular intervals (and in near real-time if appropriate). UKHSA’s COVID-19 dashboard website is an example of how this should be done across programmes, through which the public can easily access data on infection, hospitalisation, and vaccination uptake rates
Introduce a Centrally Commissioned Communication Capability
In addition to the data layer, an effective (and improved) communications layer is required to transform our supportive architecture for vaccination. A centrally commissioned communication capability should therefore be introduced, which could be modelled upon the current Covid-19 and Influenza National Booking System. The aim is to enable providers – and eventually, ‘Vaccine Collaboratives’, as advocated in this report – to choose software from a provider listed on a nationally specified framework. The minimum expectation for this capability is to enable invitation scheduling, appointment booking and preparation processes. The framework should specify that all channels, including NHS App, SMS, email and phone outreach should utilised.
Patient-and Provider-Accessible Health Records
Recommendation. Enable all providers commissioned to deliver vaccinations access to the relevant sections of a patient’s health records. Enable users to view their immunisation records. Enable joint controllership of data so that systems can provide support to GPs in the management of patient data to unlock possibilities for a greater range of providers to access to anonymised information for clearly defined use cases.
Throughout our research, many front-line staff have reflected on the missed opportunities which occur where they cannot swiftly check a patients immunisation status, inhibiting ‘opportunistic’ vaccination. Community pharmacy represents the provider which is likely to prove most beneficial in enabling access to patient records, currently managed in general practice. We have also previously discussed the benefits which may derive if those in secondary care – particularly in emergency departments are able to swiftly access a patient’s immunisation record.
A range of studies have found that patient access to electronic health records can bring clinical benefits too. 206Archana Tapuria,Talya Porat & Dipak Kalra et al., ‘Impact of patient access to their electronic health record: systematic review’, Informatics for Health and Social Care, Vol. 46, No. 2 (2021) [link]; Janine Benjamins, Annemien Haveman-Nies, Marian Gunnink, ‘How the Use of a Patient-Accessible Health Record Contributes to Patient-Centered Care: Scoping Review’, Journal of Medical Internet Research, Vol. 23, No. 1 (2021) [link] As our recent report on the future for general practice, At Your Service, suggests, the aim should be to shift to a system that offers continuity of information (and thereby supporting continuity of care) across settings.207Sean Phillips, Robert Ede & David Landau, At Your Service, Policy Exchange [link] That report also recommends shifting to a new data model, whereby liability, and management of patient records is shared between GP practices (who currently act as the sole controller) and either ICSs or NHS England. Joint-controllership – as we advocate has already been introduced in Scotland. There will also be lessons to be learned from models where patient-accessible records have already been enabled, such as Australia and Sweden (see Box 11).
Changes are afoot in England through the Citizens’ Access Programme. Some patients are already able to access their records, such as those requesting permission through accuRx’s ‘Record View’ platform, provided that a healthcare professional approves it, with patients receiving a 6-digit code via SMS.208Cora Lydon, ‘accuRx launches first national patient-centred record viewing system, Digital Health, 19 May 2022 [link] After a series of delays, it had been envisaged that from 1 November 2022, all patients over sixteen across England are scheduled to be able to view their patient records via the NHS App, with historic records added over the course of 2023.209Access to patient records through the NHS App, NHS Digital [link]. This is a GMS contractual obligation for practices.
There are important caveats to bear in mind for the rollout of this scheme. Firstly, care is required to ensure the offer doesn’t unnecessarily widen inequalities or reduce access for those that do not have the capacity to engage with health services in this way.210Felicity Knights, Jessica Carter & Anna Deal, ‘Impact of COVID-19 on migrants’ access to primary care and implications for vaccine roll-out: a national qualitative study’, British Journal of General Practice, Vol. 71 No. 709 (2021), e583-e595 [link] This will necessitate conversations around the format and settings that best meet the needs of particular user groups. Moreover, whilst we believe that most issues can be effectively mitigated, it will take time for best-practice to emerge in what is effectively a shift to the joint-administration of records. GPs for instance must be able to hide elements of the patient record (or to be specific about which individuals they feel certain information is appropriately shared) – this is vital given third-party information may be contained. It has been reported that many current IT systems are unable to enable this, thereby compromising this fundamental principle of privacy that GP surgeries are legally required to uphold (under the Data Protection Act, GPs are responsible for this information as data controllers).211Helen Salisbury, ‘Unintended consequences of open access to medical notes’, BMJ, 28 June 2022 [link] Many practices are refusing consent as a result. Both the BMA and RCGP have called for the scheme to be stalled, and for patient safety and implementation issues to be addressed before further progress is made.212David Wrigley, ‘Call to rethink citizen access programme’, BMA, 28 October 2022 [link]
Progress here will ultimately be contingent upon ensuring arrangements have been optimised at a national level: that IT systems are in place and commissioned to enable GPs to redact relevant sections of records; that change management support is in place to assist practices to make the transition and to ensure best-practice is widespread; and in some instances, automatic redactions are created. As it stands, many GP practices have had to work through many of the implementation challenges without sufficient guidance and support at a national level.213Ed Turnham, Twitter thread, 31 October 2022 12:50AM [link] Some key enablers that would make a difference would include extending The Clinical Negligence Scheme for General Practice (CNSGP) to cover data breaches, thereby providing greater assurance. Above all, the implementation of such a scheme is evidence that an expansion in analytical capabilities at national, system and local levels – as the recent Goldacre Review recommended – is needed to be able to implement such a scheme, without impacting the delivery of routine care.214Ben Goldacre, ‘Better, Broader, Safer: Using Health Data for Research and Analysis (April 2022) [link]
We believe that the principle of patient access to records is important and we would wish to see a move whereby users can input and amend their vaccination records (subject to approval by an appropriate healthcare professional), including their travel vaccinations (which are not delivered on the NHS). The Vaccine Data Resolution Service (VDRS) should be made more accessible to users to fulfil this purpose. Such an approach will be commensurate with commitments in the Government’s recent Plan for Digital Health and Care and the Integration White Paper, both of which call for the NHS App to offer a personalised experience and to encourage them to engage in tailored preventative activity (including immunisations and vaccinations). For instance, the NHS App should provide access to immunisation records beyond the COVID-19 vaccine certificate in due course.
| Box 14. Australia and Sweden: Patient Managed Electronic Health Records (EHRs) |
| Australia: My Health Records
Australia provides EHRs, called My Health Records (launched in 2012), to everyone that has either a Medicare card or individual healthcare identifier, enabling users and providers access to records. Consumers have the option to restrict access to some or all of the documents in their record. This has allowed healthcare providers across different settings and geographical areas to gather relevant information instantly, especially in the event of medical emergency. This does not replace clinical information systems at GPs or other healthcare providers at the local level. Providers can upload clinical documents, which include medicines, diagnostic summaries, e-Referrals, pathology reports, prescription, and immunisation215My Health Record, digitalhealth.gov.au [link] . Sweden: Journalen Sweden also launched its national patient accessible EHRs in 2012. Journalen gives users a single record with information from any health care provider they have visited216Maria Hägglund & Isabella Scandurra, ‘User Evaluation of the Swedish Patient Accessible Electronic Health Record: System Usability Scale’, JMIR Human Factors, Vol. 8, No. 3 (2021) e24927 [link]. However, the functionality of Journalen varies across the 21 regions and can include diagnostic test results, referral notes, and immunisation status amongst a variety of features. |
3.4. Engaging Citizens
“Currently immunisation programmes are too often designed for the convenience of service providers, not patients”
Research Participant, 2022
Recommendation. Disinformation should be tackled with the development of a permanent communications cell in the NIS, working with DHSC and DCMS. It should be modelled on the Rapid Response Unit introduced by the Cabinet Office during the COVID-19 pandemic
Recommendation. The charity and voluntary sector should work together to establish an umbrella Life Course Immunisation advocacy group.
Challenges with vaccine confidence have existed since the first vaccines were developed, but the proliferation of anti-vaccination misinformation through social media in particular has given it renewed significance.217COVID-19 vaccine misinformation, UK Parliament, 26 April 2021 [link]; Eve Dubé, Maryline Vivion & Noni E MacDonald, ‘Vaccine hesitancy, vaccine refusal and the anti-vaccine movement: influence, impact and implications’, Expert Review of Vaccines, Vol. 14, No. 1 (2015) [link]; Neha Puri, Eric A. Coomes, Hourmazd Haghbayan & Keith Gunaratne, ‘Social media and vaccine hesitancy: new updates for the era of COVID-19 and globalized infectious diseases’, Human Vaccines & Immunotherapeutics, Vol. 16, No. 11 (2020), 2586-2593 [link]; Eve Dubé & Noni E MacDonald, ‘How can a global pandemic affect vaccine hesitancy?’, Expert Review of Vaccines, Vol. 19, No. 10 (2020) [link]. See also a new report: Patrick Swain, The Digital Pandemic: Life course immunisation in an era of fake news’, Coalition for Life Course Immunisation (2022) [link] Part of the challenge lays in the quantification of the challenge: as Professor Helen Bedford has recently claimed, “we have the uptake figures, but we don’t have the attitudinal insights”.218Emma Wilkinson, ‘Is anti-vaccine sentiment affecting routine childhood immunisations?’, BMJ, 10 February 2022 [link] The reasons for ‘hesitancy’ are often complex and context-specific – something that both Policy Exchange and a wide variety of organisations found when assessing the initial stages of the COVID-19 vaccination rollout.219 Robert Ede & Sean Phillips, ‘Closing the Covid-19 data gap: Assessing the initial phase of the vaccine rollout’, Policy Exchange, 26 January 2021 [link]; VacciNation: Exploring vaccine confidence with people from African, Bangladeshi, Caribbean and Pakistani backgrounds living in England (June 2021), Healthwatch England [link]; Caitlin Jarrett, Rose Wilson & Maureen O’Leary, ‘Strategies for addressing vaccine hesitancy – A systematic review’, Vaccine, Vol. 33, No. 34 (2015), 4180-4190 [link]; Heidi J. Larson, Caitlin Jarrett & Elisabeth Eckersberger, ‘Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: A systematic review of published literature, 2007–2012’, Vaccine, Vol. 32, No. 19 (2014), 2150-2159 [link]; George Kassianos,Joan Puig-Barberà & Hannah Dinse, ‘Addressing COVID-19 vaccine hesitancy’, Drugs in Context, Vol. 11 (2022) [link] One recent study queries the usefulness of the term ‘vaccine hesitancy’ for its varied and confusing use.220Daphne Bussink-Voorend, Jeannine L. A. Hautvast & Lisa Vandeberg et al., ‘A systematic literature review to clarify the concept of vaccine hesitancy’, Nature Human Behaviour (22 August 2022) [link] We know however that building trust and ‘confidence’ is key to tackling doubt. Professor Heidi J. Larson, founder of the Vaccine Confidence Project, writes that “vaccine acceptance is about a relationship, about putting trust in scientists who design and develop vaccines, industries that produce them, health professionals who deliver them, and the institutions that govern them. That trust chain is a far more important level of acceptance that any piece of information. Without these layers of confidence, even the more scientifically proven and well-communicated information may not be trusted”.221Heidi J. Larson, Stuck: How Vaccine Rumors Start- and Why They Don’t Go Away (Oxford, 2020), p. xxiv
Figure 5. ‘Vaccine Acceptance Spectrum’
Source: Lan Li, Caroline E Wood & Patty Kostkova, ‘Vaccine hesitancy and behavior change theory-based social media interventions: a systematic review’, Translational Behavioral Medicine, Vol. 12, No. 2 (2022), 243–27 [link]
The latest guidance from the National Institute for Health and Care Excellence (NICE) provides a useful summary of further reasons that uptake may be limited222Vaccine uptake in the general population, National Institute for Health and Care Excellence, Guideline NG218, 17 May 2022 [link]. These include:
- Inflexible and inconvenient clinic times and locations
- Perceived lack of balanced information
- Language and literacy problems
- Insufficient time to discuss concerns
- Lack of staff training in how to discuss vaccination
- Uncertainty about vaccine safety and effectiveness
- Uncertainty about whether vaccinations are needed (incl. disease severity)
- Previous negative experiences of vaccination
- Lack of trust in Government, drug companies and healthcare system
- Religious or cultural views
- Individual barriers, such as needle phobia or sensory impairment
These can be grouped into several themes including accessibility, approachability and awareness.223For this 5As taxonomy, capturing “all identified determinants of vaccine uptake”, see Angus Thomson, Karis Robinson & Gaëlle Vallée-Tourangeau, ‘The 5As: A practical taxonomy for the determinants of vaccine uptake’, Vaccine, Vol. 34, No. 8 (2016), 1018-24 [link]. A WHO review also discusses these themes, see Nino Berdzuli & Siddhartha Sankar Datta ‘How to tackle inequitable access, vaccine hesitancy, and other barriers to achieve high vaccine uptake’, BMJ (2022) [link]. For a review of Tailoring Immunisation Programmes (TIP), see Eve Dubé, Julie Leask & Brent Wolff, ‘The WHO Tailoring Immunization Programmes (TIP) approach: Review of implementation to date’, Vaccine, Vol. 36, No. 11 (2018),1509-1515 [link]; Elizabeth Cecil, Lindsay Helen Dewa & Richard Ma, ‘For GP perspectives on the effectiveness of reminders, see General practitioner and nurse practitioner attitudes towards electronic reminders in primary care: a qualitative analysis’, BMJ Open (2021) [link].
Accessibility – According to a recent report from the Royal Society for Public Health, the timing, availability and location of appointments were identified as barriers to vaccination across the life course by the public and by healthcare professionals – although the vast majority of people who chose not to vaccinate do not cite inconvenience as a key factor.224Moving the Needle: Promoting Vaccination Uptake Across the Life Course, Royal Society for Public Health [link] In fact, only for influenza vaccination did any significant number of parents (according to their findings) indicate that inconvenience of accessing the vaccine was a factor contributing to their decision not to vaccinate their child, with 24 of 496 parents (5%) agreeing this was the case.225Ibid. p. 11 Older adults believed key barriers to be the availability of appointments (34% agreed) and the location of appointments (27%).226Ibid. p. 23 Research published by Public Health Scotland and the University of Edinburgh revealed that uptake of the MMR and 6-in-1 vaccine among Scottish pre-school children paradoxically increased during the first Covid-19 lockdown in spring 2020 for a range of factors which included direct communication with families to remind them of upcoming appointments and easier access to vaccination centres.227Fiona McQuaid, Rachel Mulholland & Yuma Sangpang, ‘Uptake of infant and preschool immunisations in Scotland and England during the COVID-19 pandemic: An observational study of routinely collected data’, PLOS Medicine, 22 February 2022 [link] Leveraging the Citizens’ Panel in Integrated Care Systems (ICS) alongside other patient and public involvement platforms will be of use to gauge where services ought to be delivered.
Box 15. International Best Practice: How to increase flexibility and ease of vaccination?
| Appointment Making | |
| Websites | In Sweden and Switzerland, the public can make an appointment online or through the phone. Although in Switzerland, this is dependent on the canton/sub-regions. There were wide disparities in the approach to COVID-19 vaccine rollout. |
| Apps | In Israel and Portugal, users can book vaccine appointments through an app. Portugal has a well-established app––SNS 24––that contains information on a patient’s health and provides clinical and nonclinical services. It also offers services for citizens to solve health-related issues without having to access primary care or the hospital. |
Approachability – Attempts to address service provision gaps in ways that involve trusted community organisations, and which ‘localise’ responses, including tailoring communication or implementation strategies are particularly effective.228There is a wealth of academic literature supporting the importance of enabling localised, or hyper-localised strategies as part of service delivery: Kristoffer Halvorsrud, Jenny Shand & Leonora G Weil, ‘Tackling barriers to COVID-19 vaccine uptake in London: a mixed-methods evaluation, Journal of Public Health, Vol. 44, No. 3 (2022) [link] Some scholars have described this as a ‘precision public health’ approach, which takes into account local variation, and the specific needs and circumstances of vulnerable populations.229Peter Piot, Heidi J. Larson & Katherine L. O’Brien et al., ‘Immunization: vital progress, unfinished agenda’ Nature, Vol. 575 (2019), 119–129 [link] After all, Covid-19 vaccination rates varied greatly across England, with deprivation a factor in lower uptake.230For a list, see ‘A review of research into vaccine uptake in the UK, Local Government Association [link]. On the impacts of deprivation upon uptake, see Eram A. Haider, Lorna J. Willocks & Niall Anderson, ‘Identifying inequalities in childhood immunisation uptake and timeliness in southeast Scotland, 2008–2018: A retrospective cohort study’, Vaccine, Vol. 37, No. 37 (2019), 5614-5624 [link] There are clear disparities in uptake between groups also. The ‘White British’ population was vaccinated – for instance –at significantly higher rates on average than the ‘Black Caribbean’ population.231Charlotte Hannah Gaughan, Cameron Razieh & Kamlesh Khunti, ‘COVID-19 vaccination uptake amongst ethnic minority communities in England: a linked study exploring the drivers of differential vaccination rates’, Journal of Public Health, fdab400 (2022) [link]; Judith Eberhardt, Jonathan Ling, Louis Horsley, ‘Exploring COVID-19 Vaccine Confidence with People from Black and Asian Backgrounds in England’, Journal of Racial and Ethnic Health Disparities (2022) [link]. Disparities in uptake have also been observed in Israel and Australia (two countries we have investigated closely in this report), with Ultra-orthodox Jewish and Arab populations having lower vaccination rates than the wider population in Israel; the Indigenous population persistently achieving lower coverage than other Australians across all states (see Graph 6 below).
Finding ways to target what are themselves heterogenous communities is a challenge. A recent Healthwatch England report shows attitudes toward NHS initiatives to achieve greater uptake amongst target groups from ‘African, Bangladeshi, Caribbean and Pakistani’ backgrounds. It reveals that approaches could be ineffective and even patronising if not approached sensitively and transparently.232VacciNation: Exploring vaccine confidence with people from African, Bangladeshi, Caribbean and Pakistani backgrounds living in England (June 2021), Healthwatch England [link] A recent study which considers measures to improve vaccination uptake amongst traveller, Gypsy and Roma communities (whose uptake rates are well below the national average), finds building trusted relationships; facilitating attendance at appointments; and improved record keeping and monitoring to be effective strategies for driving uptake.233Julie Mytton, Helen Bedford & Louise Condon et al., ‘Improving immunization uptake rates among Gypsies, Roma and Travellers: a qualitative study of the views of service providers’, Journal of Public Health, Vol. 43, No 4 (2021), e675-e683 [link]; Pierre Verger &Eve Dubé, ‘Restoring confidence in vaccines in the COVID-19 era’, Expert Review of Vaccines, Vol. 19, No. 11 (2020) [link]. Tailored approaches have been understood as necessary to boost uptake of HPV vaccine coverage in Muslim, Jewish schools and to reach pupils in smaller specialist schools.234Ben Kasstan, Sandra Mounier-Jack & Louise Letley, ‘Localising vaccination services: Qualitative insights on public health and minority group collaborations to co-deliver coronavirus vaccines’, Vaccine, Vol. 40, No. 14 (2022), 2226-2232 [link]
The “most potent intervention” for increasing vaccine uptake is the trusted recommendation from healthcare providers, but it is unclear whether such recommendations are effective because they increase confidence, set social norms, or reflect a direct behaviour change. It is plausible to suggest it achieves all three.235Noel T. Brewer, ‘What Works to Increase Vaccination Uptake’, Academic Paediatrics, Vol. 21, No. 4 (2021), S9-S16 [link] A pilot scheme undertaken in Liverpool in which GPs phoned patients who had declined or ignored Covid jab invitations led to more than half agreeing to be vaccinated as a result.236‘Covid: Vaccine-hesitant patients in Leicester get GP phone calls’, BBC News, 2 March 2021 [link] Out of 200 vaccine-hesitant patients called by one practice, 125 decided to go ahead with the jab after discussing their concerns with a doctor. The importance and influence of social networks is also clear, with 60% of people surveyed agreeing the opinions of friends and family were trusted and valued. When it comes to vaccination, the messenger matters, meaning that giving users the choice over who contacts them is of real importance. In most cases, GP practices will remain best placed to act as the key point of contact and should play a coordinating role in scheduling call and recall notifications.
Awareness – is about the system getting on the front-foot, ensuring that information presented to the public is accurate; that surveillance data is accessible and up to date, both of which improve confidence amongst users through improved ‘operational transparency’.237Ryan W. Buell, ‘Operational Transparency’, Harvard Business Review (March–April 2019) [link]. See Robert Ede & Sean Phillips, ‘A wait on your mind’, Policy Exchange (21 July 2021) [link] for an example of suggestions of how the concept can positively impact health service performance. Improving surveillance data is a key plank of this strategy, building confidence amongst users of the intelligence of the system.238Heather M. Scobie, Michael Edelstein & Edward Nicol et al., ‘Improving the quality and use of immunization and surveillance data: Summary report of the Working Group of the Strategic Advisory Group of Experts on Immunization’, Vaccine, Vol. 38, No. 46 (2020), 7183-7197 [link]
Bringing these features together, the results from a February 2019 study from NHS Scotland, entitled ‘Exploring public views of vaccination service delivery’ are instructive. This examined the features that those interviewed associated with creating a more approachable, and effective vaccination service.239Rachel Bishop, Alison Miller & Menekse Suphi, Exploring public views of vaccination service delivery, NHS Scotland, February 2019 [link] These features were as follows:
- Patients would be informed initially from a mix of sources that would all then feed into a central invite system: from GPs, practice nurses, hospital staff, pharmacists.
- The invitation system would be a new central system with one database held that triggered initial invitations sent on paper or email and with information included as per the invite format. All communications would be as per patient preference.
- The decision would be based on the patient having the information that makes the vaccination relevant and important to them, including why the individual should have the vaccination, the consequences if they do not, what the vaccine is, what is in it, what it does, what side effects it could have, and so on.
- Running alongside all of this would be ongoing communications promoting the vaccinations service and stating why it is relevant and needed, busting myths and promoting correct information and also giving information on how the programme is doing over time.
- The appointment must be easy to make and systems need to be created that can be accessed out of office hours, with self-booking systems and the assurance that appointments will be available with a call back or notification push if someone does need to wait for an appointment slot.
- On the day, the process would be simple for the vaccine itself, but the future would see a system that is in a ‘local to me’ location, with NHS staff that are trained well, quick and efficient, at a convenient time for the patient, by appointment or block time or drop in (only if efficient), ID verified, linked into medical records, with an information card to read at the start and sufficiently engaging that the patient feels able to ask questions if they want to.
- For aftercare there is a need to develop an aftercare information card, giving details of potential side effects, what to do and who to report them to.
Graph 6. Variation in COVID-19 vaccination uptake between societal groups, UK and Australia
Source(s): Coronavirus (COVID-19) latest insights: Vaccines, Office for National Statistics [link]; Vaccination numbers and statistics, Australian Government – Department of Health and Aged Care [link]
Improving ‘Vaccine Confidence’ Through Pro-Immunisation Advocacy
Recommendation. Organisations across the charity and voluntary (VCSE) sector should collaborate to establish an umbrella Life Course Immunisation advocacy group.
In conducting this research, it has been striking – particularly in comparison to major disease areas such as cancer or dementia for instance – how disparate advocates for immunisation are across the VCSE sector. Whilst many charities will lead specific campaigns for age-related vaccines, and the British Society for Immunology have created a wealth of useful resources, there is no clear, unified and eminent pro-immunisation advocacy voice in the public debate at present.240A guide to childhood vaccinations, British Society of Immunology [link] This is concerning because of the pervasiveness of those advocating against immunisation.
A recent study in Nature shows anti-vaccination commentary (and associated websites/ social media) tends to have fewer followers but is more numerous than ‘pro-vaccination’ sources and more often linked to discussions amongst those whose stance on vaccination is undecided.241Misinformation also travels at greater speed, Soroush Vosoughi, Deb Roy & Sinan Aral, ‘The spread of true and false news online’, Science, Vol 359, No. 6380 (2018), 1146-1151 [link]; Seth C Kalichman, Lisa A Eaton, Valerie A Earnshaw, Natalie Brousseau, ‘Faster than warp speed: early attention to COVD-19 by anti-vaccine groups on Facebook’, Journal of Public Health, Vol. 44, No. 1 (March 2022), e96–e105 [link] In contrast, sources which explain the benefits of and scientific case for vaccination are “largely disconnected from this ‘main battlefield’ for public sentiment”.15 A unified immunisation advocacy group could play a useful coordinating role, but efforts to create such an organisation have not borne fruit. A recent study from the International Federation on Ageing revealed factors limiting progress including capacity issues for VCSE organisations juggling competing priorities, and the challenge of tailoring messages accurately and appropriately across populations with a wide variety of needs and conditions.17 This health literacy factor is important and innovative solutions will be required to address current challenges. A UK Government commissioned survey of 2,000 parents suggests many are not aware of the risk measles (for instance) poses. Only 38% were aware measles could be fatal; 56% did not know that two doses were required to complete the full course. A ‘life-course’ approach will be required to counter findings from a recent study that many older people tend to associate “vaccination” with the jabs that children and babies receive, such as MMR and polio242Liam Hanson, Ready to roll out: Improving routine vaccination uptake in the UK, post-pandemic, International Longevity Centre (August 2021) [link], p. 9.
It is our view that a federation of existing Voluntary, Community and Social Enterprise (VCSE) organisations could help to ensure resources are pooled most effectively, whilst acting as a public champion and advocate for all immunisation programmes.
Tackling Vaccine Disinformation
Recommendation. Disinformation should be tackled with the development of a permanent communications cell in the NIS, working with DHSC and DCMS. It should be modelled on the Rapid Response Unit introduced by the Cabinet Office during the COVID-19 pandemic.
A main source of vaccine misinformation and conspiracy theories are groups that explicitly oppose vaccinations. A majority of those engaging with these groups express caution against trusting vaccines, doubts regarding vaccine safety and a need for ‘natural alternatives’ to vaccination and conspiracy theories implicating the government, public health advocates and pharmaceutical companies in unethical practices.243Beth L. Hoffman, Elizabeth M. Felter & Kar-Hai Chu, ‘It’s not all about autism: The emerging landscape of anti-vaccination sentiment on Facebook’, Vaccine, Vol. 37, No. 16 (2019), 2216-2223 [link] Groups are becoming increasingly adept at manipulating platforms to proliferate bogus content. A recent study, reported by the BBC, showed that anti-vaxxers used carrot emojis in place of the word “vaccine” in order to circumvent Facebook algorithmic content searches, which target words, rather than images.244‘Anti-vax groups use carrot emojis to hide Facebook posts’, BBC News, 16 September 2022 [link] Some of this activity is coordinated and international. Major anti-vaccine groups were operating weeks before the US government launched its own vaccine development program ‘Operation Warp Speed.’ In short, anti-vaccine misinformation campaigns often outpace public health messaging and have been a causal factor in hampering the rollout of vaccines.245Seth C Kalichman, Lisa A Eaton, Valerie A Earnshaw & Natalie Brousseau, ‘Faster than warp speed: early attention to COVD-19 by anti-vaccine groups on Facebook’, Journal of Public Health, Vol. 44, No. 1 (March 2022), e96–e105 [link] These communities are complex however and require tailored interventions.246Beth L. Hoffman, Elizabeth M. Felter & Kar-Hai Chu, ‘It’s not all about autism: The emerging landscape of anti-vaccination sentiment on Facebook’, Vaccine, Vol. 37, No. 16 (2019), 2216-2223 [link]
This ‘infodemic’ – as one paper describes it – requires sustained effort in Government so it can be effectively tackled.247Nicky C Cardenas, ‘Europe and United States vaccine hesitancy’: leveraging strategic policy for ‘Infodemic’ on COVID-19 vaccines ‘, Journal of Public Health, Vol. 44, No. 2 (June 2022), e315–e316 [link] One recent web-based study of 600 adults in Florida found high levels of vaccine misinformation among participants, with 73% reporting some exposure to misinformation about COVID-19 vaccines in the past six months. This exposure was directly correlated with vaccine hesitancy. Among those who did not report any exposure to misinformation, 73.8% were vaccinated. That number fell to 62.9% with exposure to just one misinformation theme and 52.2% for six or more.248Stephen R. Neely, Christina Eldredge, Robin Ersing & Christa Remington, ‘Vaccine Hesitancy and Exposure to Misinformation: A Survey Analysis’, Journal of General Internal Medicine, Vol. 37 (2022), 179–187 [link]
This issue therefore requires strategic and targeted messaging on the part of health and care professionals. During the COVID-19 pandemic, a Rapid Response Unit, operating from within the Cabinet Office and No10, tackled a range of harmful narratives during COVID- from purported ‘experts’ issuing dangerous misinformation and coordinated with departments across Whitehall to deploy appropriate responses.249Government cracks down on spread of false coronavirus information online, gov.uk, 30 March 2020 [link]
This included direct rebuttal on social media, working with platforms to remove harmful content and ensuring public health campaigns are promoted through reliable sources. The unit fed into the wider Counter Disinformation Cell led by the Department for Digital, Culture, Media and Sport, made up of experts from across government and in the tech sector.
We foresee a permanent comms cell being developed by the NIS which could feed into DCMSs Counter Disinformation Cell moving forward. It would engage closely with the life course advocacy organisation, detailed above, in the creation of assets and information to counter false and misleading narratives.
Developing a Vaccine Registry
Recommendation. The Government should further support NHS England and the NIHR to drive interest and user engagement (as well as NHS partnerships with the life sciences sector) by creating a comprehensive Vaccine Research Registry, modelled on the COVID 19 Vaccine Registry
The COVID-19 NHS Registry attracted 550,000 people to sign-up since it launched in the Summer of 2020, with about 50,000 engaged in 18 different vaccine trials for seven different companies. Over a third of the registry members are over 60, groups at particular risk from COVID infection.250Roger Highfield, Coronavirus: How the UK Backed Vaccine Winners, Science Museum, 22 February 2021 [link] Recent reporting had suggested the Registry’s future was under threat, but, the Rt Hon Robert Jenrick MP, the former Minister of State for Health used external legal advice to convince civil servants it would not breach data protection laws if volunteers who had signed up to the original COVID Registry were asked to take part in other medical studies.251Kate Bingham, Tweet dated 23 August 2022 11:55 AM [link]; Chris Smyth, ‘Covid database revived to fight other diseases’, The Times, 26 October 2022 [link] The NHS and the NIHR have an opportunity to boost partnerships with the life sciences sector further, by ensuring the Registry encompass research into vaccines across the life course (as well as a host of other disease areas), and continuing to deliver upon the promise of increased user engagement alongside the benefits to UK Plc, that the Covid-19 Registry demonstrated.
Further Leveraging the NHS App
Recommendation. Additional functionality should be added to the NHS App, ensuring the availability of high-quality information, and options to book immunisations. For parents, consent and broader child health information (a digital or e-red book) should also become more readily accessible.
Commitments in the Government’s recent integration white paper calls for the NHS App to offer a personalised experience and to encourage users to engage in tailored preventative activity (including immunisations and vaccinations) 252Health and social care integration: joining up care for people, places and populations, gov.uk, 9 February 2022 [link]. It also builds on the commitment made by the former Secretary of State for all COVID vaccinations to be bookable via the App by March 2023 – so that service users (or relevant nominated persons) can access their full ‘life course’ immunisation record, as well as to book and manage immunisation appointments.
E-Consent
E-consent for childhood and school age immunisation should be offered to parents and carers where appropriate. Sharon White of the School and Public Health Nurses Association (SAPHNA) has stated that “many areas still have archaic systems, including paper-based, which bring huge issues and barriers. E-consent (electronic) systems are necessary to ensure maximum efficiencies, safety, and uptake.”253Delivering a school-based immunisation programme and maintaining uptake in the context of the COVID-19 pandemic, British Journal of Child Health, Vol. 1, No., 5 (2020) [link]
E-Redbook
The development of a digital, or an electronic ‘red book’, inspired by the paper-based version – first introduced in the 1960s for parents to log child health information from infancy to four years of age – has long been an aspiration. The aim of this digital version is to enable the creation of a ‘one stop shop’ for parents, with reminders issued at key milestones and for accurate and NHS-approved information to be available at a parent’s fingertips. An Early Year’s review from the Government, entitled, The best start for life: A vision for the 1,001 critical days listed Digital Personal Child Health Record within its vision.254The best start for life: a vision for the 1,001 critical days, gov.uk, 25 March 2021 [link] A commitment was also contained in the 2019 Long Term Plan: that by “2019/20, 100,000 women will be able to access their maternity record digitally with coverage extended to the whole country by 2023/24.” So far, the initiative, developed as part of the Digital Child Health Transformation Programme with NHS England and the Royal College of Paediatrics and Child Health has enabled the development of version which has been rolled out across London and Essex.255eRedbook, North East London NHS Foundation Trust [link] It has yet to scale however to other regions, however with uptake variable and often defined by professional buy-in.
As part of this research, it has become clear that a number of developments are required to expand this offer. Firstly, a national commissioning model is required so that developers have a clear sense of technical and content requirements as well as clear partners to deliver the service. This should be coupled with a new approach to content management for materials relevant to children’s health at large. Key stakeholders from NHS England (including representation from S7a team), OHID and Royal Colleges should be brought together to determine what should feature in this single portal – it may be appropriate for a steering group to be established for this purpose. The current ‘Birth to Five’ resource for instance – we believe –should be embedded.256Digital revolution to bust COVID backlogs and deliver more tailored care for patients, Gov.uk, 29 June 2022 [link] The aim however, is to create a single, effective portal for parents or carers.
3.5. Assessment and Regulation
“People are always saying that the JCVI should be more like NICE. But these comparisons feel hackneyed. The JCVI role is more complex. The Committee is making population-wide recommendations, often having to absorb and synthesise enormous uncertainty. And their work is supported by a threadbare secretariat of a few people”
Semi-structured interview, 2022.
“All the members are unpaid and originally sign up to three meetings a year. But since December 2020 the Committee has met more than 100 times”
Semi-structured interview, 2022.
The Joint Committee on Vaccination and Immunisation (JCVI) and capacity to assess new vaccine technologies
Recommendation. Several reforms should be taken forward to modernise the approaches and workings of the Joint Committee on Vaccination and Immunisation (JCVI) which should be reflected in Code of Practice.
These reforms would attempt to mimic elements of NICE, which has a strong predictive arm, an underlying commitment to transparency, and a mature relationship with industry dialogue, whilst recognising the unique strengths of the JCVI.
The recent Life Science Vision considers how the UK can strengthen its position as a world leader in the development, testing, access, and uptake of new and innovative treatments and technologies. In particular, to sustain its position in vaccine discovery, development and manufacturing.257Life Sciences Vision, gov.uk, 6 July 2021 [link] Yet industry partners have expressed concerns about the speed of National Immunisation Technical Advisory Group (NITAG. In the UK, JCVI) decision-making, procurement and rollout of proven products. A study revealed that about half of the fifteen European countries studied reported the process from NITAG recommendation and programme roll-out takes more than six years.258Valérie Laigle, Maarten J Postma & Mira Pavlovic, ‘Vaccine market access pathways in the EU27 and the United Kingdom − analysis and recommendations for improvements’, Vaccine, Vol. 39, No. 39 (15 September 2021), 5706-5718 [link] The UK falls within this category; the other half have an average duration of less than six years.
The JCVI is the independent committee that assesses new vaccines and advises Ministers of Health on preventative vaccine policy. Initially established as an advisory board for polio immunisation in 1963, it became a statutory organisation as the Standing Advisory Committee on vaccination and immunisation in 1981 and was reconstituted as a departmental expert committee in 2012.259For a useful short history of the JCVI, see Andrew J. Hall, ‘The United Kingdom Joint Committee on Vaccination and Immunisation’, Vaccine, 28S (2010) A54–A57 [link] Its members, which currently numbers sixteen including paediatricians, respiratory physicians, virologists and general practitioners routinely meet and report as a committee three times a year, the contents of which are released in the form of minutes which summarises key decisions and recommendations on its website, and its recommendations published in “immunisation against infectious diseases” guidance to clinicians.260It should be noted that recent commitments have far exceeded this, with the total number of meetings over the past eighteen months well over 100. Membership is voluntary and unpaid. The JCVI’s role is crucial as it assesses evidence on the safety, cost, and quality of new vaccines before they are introduced to the national immunisation programme that would affect a large proportion of healthy population. Unlike most expert committees, the advice of the JCVI is requested by Ministers and they are legally obliged to implement its formal advice. If the JVCI reviews evidence and recommends a particular course of action which differs from what the regulator (Medicines and Healthcare products Regulatory Agency, or MHRA) has approved for the product licence (such as recommending a change to the number or timing of doses), its recommendations can ‘outrank’ the licence (or, as with the COVID-19 vaccines, their Emergency Use Authorisation).261Peter M.B. English, The UK approach to COVID-19 vaccination: why was it so different?, Drugs in Context, Vol. 10 (2021) [link]
Transparency in decision-making
The robust nature of the expert-led, committee decision making process was held up by several of our interviewees as a distinguishing factor of the JCVI. These fundamentals are strong, ‘world-leading’ even. Any reforms must safeguard what is working well, and this report makes no recommendations that would lead to a major deviation in the core structure of the JCVI.
However, some interviewees did suggest that whilst not doubting the independence of the decision-making process, the decision architecture could itself be more transparent and standardised. Compared to the National Institute for Health and Care Excellence (NICE) which provides technology appraisals on medicines, the JCVI does not typically explain its process or provide a timeline of its decision-making. As well as providing assurance to manufacturers, being able to communicate its process is crucial to gaining and maintaining public confidence. NICE publishes full appraisal reports including associating documentation to justify Health Technology Assessment decisions. Whilst models often are published by the JCVI, these do not necessarily neatly align with the timing of the decision (sometimes with a substantial lag). This can mean that manufacturers have a limited understand behind the decision-making progress and it can remove the possibility for informed external scrutiny. JCVI also does not publish its cost-effectiveness model. In some instances, this has been seen as a limitation to its approach given that tenders for vaccine procurement are based on the result of cost-effectiveness study. The tender criteria and technical reports are not routinely published, which begs the question of what criteria are used to decide which reports get published and which remain confidential. As an expert committee, JCVI does not have a citizen council to review elements of the institute’s methods, procedures and decision-making, which provides a platform for public scrutiny and opinion. Currently one layperson sits on the Committee, with a recruitment process underway to fill the second vacant layperson position.
Direct comparisons between the resource and capabilities of the JCVI and NICE can often feel misplaced. NICE has an FTE headcount of 807; the JCVI secretariat only has five. If the JCVI is to be expected to develop the horizon scanning capabilities recommended in this report, more investment is needed to support evolutionary change. The objective of this exercise should be to boost the organisational resilience, to ensure that the secretariat function can fully support the experts on the respective committees, and to develop the JCVI’s methods and processes to maximise the positive learnings from the pandemic. This is necessary to enable the JCVIs capabilities to flex sustainably as and when required in the case of clustering of new programmes or where future outbreaks, epidemics, and pandemics occur.
When looking at international best practices, the NITAGs of Australia and Israel provide digital access to committee minutes, with Israel including the names of speakers. NITAGs in Portugal, Sweden and Switzerland do not share their meeting notes (see Box 13). A technical report conducted by the European Centre for Disease Prevention and Control (ECDC) surveyed 26 countries, finding only six out of 26 countries published minutes online, including the Czech Republic, Denmark, Germany, Latvia, and the UK.262Current practices in immunisation policymaking in European countries, ECDC (March 2015) [link] Of the 26 countries, only two––Latvia and Slovenia––involve the public in meetings. This suggests that the JCVI is comparatively transparent in its decision-making, and the limited role of public’s involvement in immunisation assessment is commonplace.
Communication
The JCVI was instrumental throughout the pandemic in making a series of bold decisions including recommending variation from manufacturer recommendations in extending the ‘prime-boost’ interval between the first and second doses of the AstraZeneca and Pfizer-BioNTech vaccines. These decisions were “controversial at the time but have contributed enormously to the effectiveness of the vaccination programme”.263Peter M.B. English, The UK approach to COVID-19 vaccination: why was it so different?, Drugs in Context, Vol. 10 (2021) [link] The JCVI was praised for its effective communications in explaining its decision-making during the pandemic, which included frequent statements to update its decisions, and holding news briefing on media and press.
There are however, elements of the way in which it communicates its decisions which could be strengthened. One example is the way in which is communicates anticipated transitions from “older” to “newer” vaccine technologies. Were the JCVI to implement a more formal set of “horizon scanning” activities (as this report encourages), ensuring there is clarity on how JCVI the anticipates use by providers of multiple vaccine platforms will be beneficial. Clearer guidance could enable more accurate production expectations from industry.
Horizon-scanning and engagement with stakeholders
In terms of horizon scanning and stakeholder engagement, the JCVI could benefit from adopting some learnings from NICE’s approach where manufacturers are involved at the preliminary stages of product licensing in a formalised and standardised process. Early advice from the relevant body is crucial for acceleration of the access pathway. In the UK, horizon scanning is routinely conducted once per year, with the JCVI often providing informal early advice. A few European countries including Denmark, France, the Netherlands, Poland and Portugal, have formalised this process, which involves either their expert committee or licensing body assessing whether a vaccine is eligible for the process, documentation, timeliness and in some cases charging a fee.264Current practices in immunisation policymaking in European countries, ECDC (March 2015) [link]
In response to these challenges, a dedicated ‘Horizon Scanning Sub-Committee’ could be established, with a remit to look up to ten years ahead (the current horizon scanning process looks at vaccines in development over the next three-five years). The sub-committee should also be encouraged to ‘direct the horizon’ with demand signalling mechanisms which determine the nationally significant vaccine-preventable diseases. Representation on the sub-committee should include epidemiologists but may also draw upon the input of representatives from the Accelerated Access Collaborative, BEIS, DHSC and NHS England.
The value of horizon scanning will assist the JCVI in planning its workload, as well as informing modelling requirements. But enhancements would support the wider ecosystem too, enabling NHSE to anticipate future roll outs (and plan for any relevant contractual changes). From the perspective of DHSC, improved horizon scanning could also enable improved budget forecasting with a longer-term view of when and how much it will seek from Treasury.
This could be accompanied to refreshed methods of engagement with manufacturers, with routes created to allow for informal two-way dialogue, supplementing the existing company days. Dialogue with the industry would support our proposed vision for JCVI to actively ‘direct’, instead of passively ‘scan,’ the horizon and achieve the UK Life Science Vision to shift towards a ‘mission-led,’ approach to the biggest healthcare problems.
To achieve this objective, additional resource will be necessary. Currently, the JCVI has no set budget.265Joint Committee on Vaccination and Immunisation: Finance – Question for Department of Health and Social Care, UIN HL14789, tabled on 12 April 2021, Hansard [link] Members are unremunerated, and only able to claim reasonable expenses. The secretariat function is effectively loaned by UKHSA. Policy Exchange believe there are some advantages to setting an annual budget for the JCVI. This would allow an expansion of the secretariat headcount, with new hires to strengthen expertise in communications, horizon scanning, stakeholder engagement, and modelling. Within this new annual budget, the JCVI should also be allowed to commission research. This should however be caveated, given there are discrepancies year-by-year in the demands the JCVI manages. Measures to enable this budget to flex, were another pandemic or outbreak to occur would have to factor in any decision.
A clear timeline for the assessment of new vaccine candidates including a process chart which should be formalised and published on the JCVI website (see Case Study in Australia, Box 17), as currently JCVI does not operate around a standardised timeline for vaccine assessment and stakeholder engagement. We expect that this transformation would minimise the process time and improve the efficiency of vaccine assessment, which is crucial for the UK to maintain its world-leading status in vaccine research.
The aim of these reforms overall, it to create an approach which enable the wider system to adapt service pathways appropriately as new vaccines enter the market, so that patients can receive rapid access once a timely JCVI decision has been made.
Bringing these recommendations together, the JCVI’s Code of Practice should be updated to reflect the evolutionary nature of these reforms.
| Box 16. Case Study: Australian Technical Advisory Group on Immunisation (ATAGI) – Horizon-Scanning and Industry Engagement |
| ATAGI has a standardised horizon scanning schedule (three cycles per calendar year). Sponsors must request a pre-submission advice from ATAGI before a vaccine submission to the Pharmaceutical Benefits Advisory Committee. ATAGI charges for services, with fees ranging from AUD $103,500 for simple cases to $181,500 for complex ones. The calendar with detailed steps and key dates are published online266ATAGI, ‘ATAGI request for pre-submission advice – information for sponsors, 2021 [link], with information such as detailed guidelines and procedures on submission available on the website; dates at which draft of meeting outcomes and final endorsed advice can be expected; templates for the pre- and final submission. Sponsors can also meet with ATAGI to seek feedback on submission plans prior to making a request for ATAGI advice.
ATAGI has several horizon-scanning methods. These include presentations by vaccine manufacturers at an annual ATAGI Industry Day, reviews of literature and decisions by regulatory authorities in other countries, and Therapeutic Goods Administration (TAG) (Equivalent of MHRA in the UK) advice to ATAGI regarding new applications for registration. Calendar of ATAGI Pre-Submission Advice Source: ATAGI, ‘ATAGI request for pre-submission advice – information for sponsors, 2021 [link] |
| Box 17. International Best Practice: The Equivalent of the JCVI in Comparator Countries (National Immunization Technical Advisory Groups, or NITAGs) | ||||||||||||||||||
|
Next chapter
Conclusion – The Future of Immunisation in England
“It is a race we are still running, ‘mutant’ variants threaten to ‘escape’ the vaccines and treatments we have developed to bring the pandemic under control. And, if and when we do cross the finishing line, sadly there will not be much time for celebration. We will already be in training for the next one.”
Sarah Gilbert & Catherine Green, Vaxxers: The Inside Story of the Oxford AstraZeneca Vaccine and the Race Against the Virus (London, 2021)
In this research we have sought to achieve a balance between reform of and support for existing immunisation policy. Too often there is a temptation to propose major structural reform, or further resources and capacity, but not both. Our paper intends to offer a balanced set of ideas that draw upon the specific assets that exist in places, the deep experience and expertise in immunisation across primary care, and the opportunities for national, high-impact enablers. This is reflected in the recommendations. A set larger than we would typically wish to include – but it reflects the multi-dimensional, and multi-agency nature of vaccination and immunisation policy. Some – including the piloting of new payment models and Vaccine Collaboratives – will take several years to implement. Others – such as moving towards a process of joint controllership of patient data or making the JCVI processes more transparent – could happen sooner. All would unlock significant benefit.
For the vaccines community there has been so much to celebrate from the past two years. A combination of scientific endeavour, sophisticated manufacturing capability, and intelligent rollout design and delivery has charted our course out of the pandemic. The challenge is to find a way of mimicking these good fundamentals in ‘peacetime’, and with a different set of vaccine-preventable diseases – some of which lack the infectiousness or severity of COVID-19 but still carry a significant burden.
This is no time for complacency. The return of polio and emergence of monkeypox demonstrate the fragility of our public health system and the close interdependency between our immunisation coverage rates and wider NHS performance. Already the UK Government has faced criticism for its monkeypox response, including the decision to not procure extra vaccine doses in the early autumn. Further outbreaks of measles, or influenza could also place major stress on routine activity this winter. In Chapter Two we outlined the impact of the slow catch-up on both measles and shingles. In 2018 a flu spike led to the wholesale cancellation of all planned operations in the NHS. With the waiting list 65% bigger in 2022 and intense political pressure to address the backlog, policymakers must not make the same mistake.