The following five entries have been shortlisted as finalists for this year’s Wolfson Economics Prize. The Judging Panel marked entries from more than 250 organisations representing 15 countries across the world, including submissions from NHS trusts, architectural practices, clinicians and patients.
The Judging Panel have also recognised three ‘Highly Commended’ entries and have made two ‘Light Bulb’ awards, recognising particularly innovative elements contained in submissions.
The five finalists will have until the end of October 2021 to expand and refine their submissions, before an overall winner will be announced in November 2021.

“The entries to this year’s Wolfson Economics Prize have been remarkably impressive. They represent examples of brilliant thinking, the world over, about how better to serve patients and support staff in hospitals. Out of an exceptionally strong field, the shortlisted entries demonstrate particularly ingenious approaches. With a renewed focus on hospital building in the UK, these finalists have a really exciting opportunity to shape how NHS hospitals look, feel and function.”
Lord Kakkar,
Chair of the Judging Panel
 Description
DescriptionA hospital design which draws upon neuroscience and the symmetry and shapes found in nature. The entrants argue this can lead to a complete rethink of hospital design, turning them from “factories for fixing” to “places for healing”.
 Description
DescriptionA multi-sensory, green hospital design, inspired by “the adaptive qualities of living systems found in nature”.
Ab Rogers Design
Advisory Group
Designers
Engineers
 Description
DescriptionA reimagination of the emergency department. It proposes innovations to reduce crowding in A&E – including First Class Airline-style pods for patients with less serious conditions.

Description
A vision for the hospital of the future, with the facility imagined as “being the community”. They propose six guiding principles: people-centric; adaptable; sustainable; technologically smart; value for money; civic and community beacons. The entry is written in the form of a a play in four Acts called The Caring Collective. The characters range from a child patient to a psychiatric nurse and are based upon real-world interactions and interviews
Entrants
Description
A hospital imagined as a virtual space with physical outposts. Proposes high-tech clinical spaces with multi-functional modular areas distributed around the hospital campus and wider community. Acute care is coordinated remotely, with a central hub providing intensive care, specialist treatment and social care to a small group of patients that have specific needs.
Entrants
Co-Authors
Samantha Field
Nick Culley
Additional Contributor:
Jenya Andersson
Description
Proposes a hybrid physical and digital ecosystem, underpinned by Healthcare Ecosystem Architecture Leadership (HEAL). Their ESSENCE design framework encourages collaborative, human-centric, biophilic and sustainable design
Zaha Hadid Architects
Patrik Schumacher, Principal
Manuela Gatto, Director
Shajay Bhooshan, Senior Associate
Yevgeniya Pozigun, Associate
Shao-wei Huang, Senior Associate
Uli Blum, Consultant
Lorena Espaillat Bencosme, Strategic Space Planner
Arjun Kaicker, External Consultant
desM
John Marsh, Director
AtelierTen
Meredith Davey, Director
WT Partnership
David Hudson, Director
Rubicon Health Consulting
Andy Whiting, Director
Design Computation Ltd.
Abel Maciel, Principal
Light Bulb Awards recognise originality and particularly innovative ideas contained within submissions.
Description Proposes to repurpose vacant major retail stores in cities and towns as outpatient and diagnostic hubs – using Sheffield and its former Debenhams store as a test case. Entrants Authors Jim Bell – Arup Edith Blennerhassett – Arup Rebecca Chau – Arup Chris Green – Arup Steve Haake – Sheffield Hallam University Agostino Nickl – Arup Helena Parsons – Sheffield Teaching Hospitals Derek Roberts – Arup Andrew Rolf – Arup Anna Sutherland – Arup Contributors Arup Foresight Team Tom Bridges – Arup Greg Fell – Sheffield Director of Public Health Jonathan Guest – Sheffield City Region Edward Highfield – Sheffield City Council Kathryn Thomas – QMC Various conversations with Staff at Sheffield Teaching Hospitals
Description A plan to promote better integration of biomedical and psychosocial models of medical care. Their concept of a community hub provides an area within the hospital where community, charity, and social care services are brought together into a collaborative space dissolving siloes and enhancing the efficiency of care provided to patients. The inter-digitation of community and hospital services promotes a rethought model of medicine which values whole-patient and personalised approaches to care. The hub model offers opportunities for health education and public engagement, emphasising a transition of the hospital from a place of cure, to a centre of prevention and health improvement. EntrantsDr Cian Wade, Academy of Medical Royal Colleges Dr Harrison Carter, NHS England and NHS Improvement Mr Thibault Quinn, Department of Architecture & Civil Engineering, Bath University
Since 2011, the Wolfson Economics Prize has created a platform for fresh thinking which can challenge orthodoxy in economics and public policy. Entry is free and open to anyone, with the winner receiving £250,000. The deadline for First Round Entries to the Prize has now closed.


“This Prize wants to draw on innovation from around the world, to help create hospitals that work better for patients, their staff and the communities they serve.”
Lord Wolfson

How would you design and plan new hospitals to radically improve patient experiences, clinical outcomes, staff wellbeing, and integration with wider health and social care?
Entrants are asked to explore this question in detail in a submission of up to 10,000 words (plus a non-technical summary of 1,000 words). Entrants can also include charts, drawings, maps, tables, links to multimedia assets, etc and are welcome to add Appendices containing ancillary material. Entries should be unconstrained by scale: it is equally acceptable to focus on one element of the hospital as to consider the facility in its entirety. However, in preparing their responses, entrants are strongly encouraged to show how their submission can address the four following areas.
Entrants are encouraged to identify specific issues in the current hospital model and then propose solutions which will lead to improvement in the experience of patients and visitors. For example, how does effective ward and room design minimise noise, reduce stress and maintain dignity whilst ensuring patients do not become isolated? How could greater use of green space and planting accelerate recovery times? To what extent does the aesthetic appearance of a hospital matter to the end user, and if so, how might it be enhanced?
Submissions should demonstrate how effective design and planning can underpin improved clinical outcomes. For example, would the physical separation of emergency and non-urgent elective surgery benefit both groups of patients? What types of facilities would be required to make this feasible within the NHS? We also know that technological advances such as robotics, artificial intelligence and remote medicine are changing the way in which care is delivered and cannot be ignored. How will new clinical services and techniques impact on future hospital design? Does modular design offer an answer? Is it possible to plan for the unknown? We would also welcome suggestions that improve infection control in hospitals and enhance patient safety.
There is evidence that a well-designed and functioning building can assist staff to perform in their roles. Designing floorplans so that doctors and nurses can move through the hospital with ease, incorporating communications and monitoring equipment as part of the build stage, and introducing on-site laboratory facilities to fast-track results are some examples of this. Alongside delivering against its primary functions, hospitals must also be welcoming work environments. This encompasses a range of considerations for staff, including transportation links, the availability of shower and locker facilities and access to green spaces. We also need to acknowledge that hospitals are 24hr buildings. How can we ensure that the hospital workforce has access to high quality food and rest facilities throughout the day and night?
The benefits of a well-functioning hospital are not restricted to the site alone. We would welcome submissions which explore how planning can achieve better integration between hospital-led and non-hospital NHS and social care services. As the boundaries between primary, secondary and tertiary services increasingly blur, do we need to rethink the notion of a hospital as a building and instead re-define it as a set of services? Another approach could look beyond the commissioning of services, and instead assess the role of hospitals as anchor institutions which foster knowledge sharing, such as through co-location with science and research. Is it feasible for hospitals to become centres of prevention as well as cure – moving our health system from orientating solely around managing illness towards promoting health?
Alongside the four priorities listed above, the Judges would welcome ideas which can be delivered in an environmentally sustainable way.
Entrants should be emboldened to think radically about what the hospital should be in the decade ahead. The Judges welcome entrants from anywhere in the world but are seeking solutions which could be applied to the health service in the United Kingdom. We encourage submissions from all parts of the community and would particularly welcome submissions from cross-disciplinary teams.
Detailed financial modelling is not expected, but submissions should nonetheless demonstrate how their idea(s) could be delivered within a normal capital envelope for new hospitals, or alternatively quantify the benefits of exceeding normal budgets.
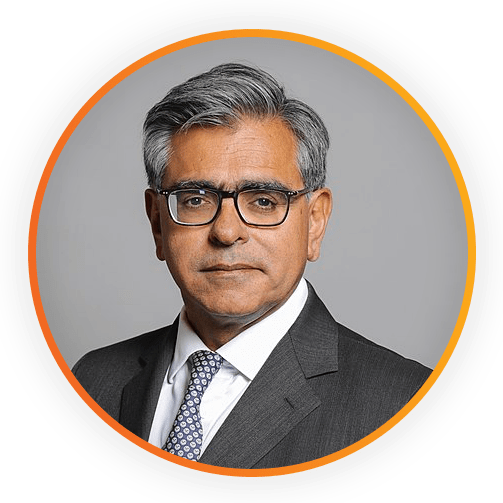
The Rt. Hon. Professor the Lord Ajay Kakkar PC is Professor of Surgery, University College London, Chairman of UCLPartners Academic Health Science Partnership and Director of the Thrombosis Research Institute London.
Lord Kakkar completed his medical degree at King’s College London and received his PhD from Imperial College London. His research interests include the prevention and treatment of venous and arterial thromboembolic disease and cancer associated thrombosis.
Lord Kakkar was created a Life Peer in 2010 and sits on the crossbenches of the House of Lords. He was Chairman of the House of Lords Appointments Commission from 2013–2018. He is Chairman of the Judicial Appointments Commission and was appointed a member of Her Majesty’s Most Honourable Privy Council in 2014. He serves as Chairman of The King’s Fund and Chairman of UK Biobank.

Dr. Brian Donley is CEO of Cleveland Clinic London – a 184 bed acute hospital, with 29 ITU beds, opening in January 2022. Cleveland Clinic will also open a state of the art outpatient building in central London in September 2021.
Prior to this appointment, Dr. Donley was Chief of Staff and Chief of the Clinical Enterprise for the Cleveland Clinic Health System. Previously, he served as President of Regional Operations for the Cleveland Clinic Health System.
Dr. Donley is Professor of Surgery at the Cleveland Clinic Lerner College of Medicine and Fellow of the Royal College of Surgeons. He attended the University of Notre Dame and graduated with Distinction from the University of Michigan Medical School. He completed the Advanced Management Program at Harvard Business School.

Dame Elaine Inglesby-Burke is a non-executive director at the National Institute for Health and Care Excellence (NICE) and former Group Chief Nursing Officer at Salford Royal Hospital and the Northern Care Alliance Group, with over forty years’ experience and service in the NHS.
Nationally, she has been recognised as an advocate for patient safety and safe nurse staffing. She was a member of the Nursing and Care Quality Forum and was an influential voice on the Berwick National Advisory Group on the Safety of Patients in England.
In 2015, she was awarded a CBE for services to nursing and in 2019, NHS England’s first national Chief Nursing Officer’s (CNO) Gold Award for Nursing. In 2020, she was awarded a Damehood in the Queen’s Birthday Honours List.

Laura began her career working as a clinical nurse specialist in Edinburgh, where she administered chemotherapy to Maggie Keswick Jencks, before becoming the first Chief Executive of Maggie’s, a role she continues to the present day. Laura shared Maggie’s vision of a cancer support centre housed in a non-clinical and uplifting environment where anybody affected by cancer could visit to access practical information, psychological and emotional support to help them build a life beyond a cancer diagnosis. There are now 26 centres with plans for future centres both in the UK and overseas. In 2016 Laura was awarded an Honorary Degree of Doctor from Queen Margaret University, and in 2019 was awarded a Damehood in the Queen’s Birthday Honours list.

Robert A.M. Stern, practicing architect, teacher, and writer, is the Founder and Senior Partner of the internationally acclaimed Robert A.M. Stern Architects, a firm with an extraordinarily diverse portfolio that has been pivotal in reintroducing respect for tradition to contemporary practice. Mr. Stern served as Dean of the Yale School of Architecture from 1998 to 2016, and in 2017 was honoured with the Topaz Medallion, awarded jointly by the American Institute of Architects and the Association of Collegiate Schools of Architecture in recognition of outstanding service to architectural education. He was the 2011 Driehaus Prize laureate and in 2007 received the Athena Award from the Congress for the New Urbanism. Mr. Stern and his firm have designed numerous buildings across the United States for healthcare and healthcare professional education.

Nigel joined Legal & General in 2009 as Group CFO, appointed Group CEO in 2012.
He is a current advisor to the Government’s Social Care Green Paper and Life Sciences Industrial Strategy Implementation Board and is Chair of the Bank of England’s Climate Financial Risk Forum, Innovation Working Group.
Nigel was a member of the Prime Minister’s Business Advisory Group (2015-2016), Chairman of the Investment Association’s review of Executive Pay (2016-2017) and the Government’s review of Mission Led Business (2016- 2017). He was also a member of the Government’s Patient Capital Review Industry Panel (2017–2018) and Commissioner in Resolution Foundation’s Intergenerational Commission (2017–2018)

Simon Wolfson graduated with a law degree from Trinity College, Cambridge.
He started working for Next in 1991 as a Sales Assistant and joined the Board as Sales and Marketing Director in 1997. In 1999 he was made Managing Director and was appointed Chief Executive in August 2001. Since he became Chief Executive Next shares have outperformed the FTSE 100 index by more than 500%.
Simon has always had an active interest in economics and politics and was created a Peer in May 2010.

Designing the Hospital of the Future
Date: 23rd March 2021
How Could Enhanced Hospital Design Boost Staff Wellbeing and Productivity?
Date: 20th May, 2021
How can our hospitals promote positive behaviours?
Date: 9th June 2021